The advent of antibiotics turned Lemierre's Syndrome into "the forgotten disease." But this easily misdiagnosed condition can potentially be fatal.
A 29-year-old man with no past medical history presents to the ED with 1 week of right-sided dental pain and new onset facial swelling. He was seen in the ED of a different hospital earlier in the week and had been started on oral penicillin for a dental infection. Initial physical exam on this repeat ED visit is notable for right mandibular/sub-mandibular swelling and tenderness, significant trismus, and jaw malalignment. Initial vital signs are as follows: Temperature 101.1 degrees Fahrenheit, heart rate 101, blood pressure 131/84, oxygen saturation 100 percent on room air. Labs and blood cultures are obtained, notable for acute kidney injury and leukocytosis. Antipyretics, IV fluids, and broad-spectrum antibiotics are administered. Bedside ultrasonography (Figure 1), is concerning for a non-compressible right internal jugular vein. Contrast-enhanced computed tomography (CT) of the neck is concerning for multiple complex periodontal, submandibular, and masticator space abscesses, with associated thrombosis of the internal jugular vein (Figure 2). Consultations to oral and vascular surgery are placed, and the patient is admitted to the hospital for continued care.
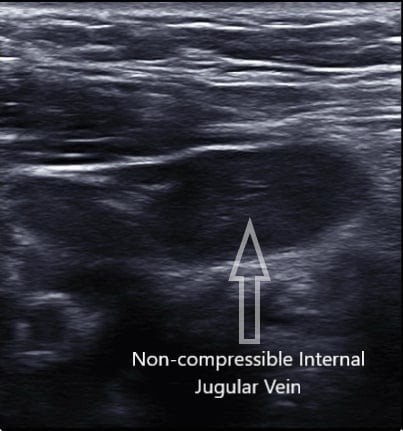
Figure 1. Bedside ultrasound of the patient's neck showing a non-compressible internal jugular vein, concerning for thrombosis

Figure 2. CT neck with contrast showing: A) one of many abscesses; B) loss of patentcy of internal jugular vein, concerning for thrombosis
Discussion
Lemierre’s syndrome was first described by French bacteriologist André Lemierre in 1936. In his landmark publication, On Certain Septicaemia Due to Anaerobic Organisms, he eloquently describes the condition as an “anaerobic postanginal septicaemia,” and found that it classically, and interestingly, afflicts previously healthy, young adults.1 Historically the disease is also termed the “forgotten disease,” after its steep decline in incidence following the advent of antibiotics.2 While only affecting 1 in 1 million patients per year, a misdiagnosis could potentially be fatal.
Today the condition is defined as a septic thrombophlebitis of the internal jugular vein due to an adjacent deep-space neck infection. On history and exam patients with Lemierre’s can have fevers, rigors, odynophagia, neck pain/tenderness, swelling, limited range of motion of the neck, and perhaps the pathognomonic “cord sign.” This is seen in less than half of cases, and characterized by pain and swelling along the sternocleidomastoid muscle.3
Infections are nearly universally oropharyngeal in origin and disseminate via direct extension towards the carotid sheath. Patients frequently present to the ED appearing clinically ill, requiring aggressive resuscitation and treatment for sepsis. Management often requires definitive surgical treatment of the primary infection.4
Complications from Lemierre’s syndrome include persistent bacteremia, septic shock, and septic emboli to joints or lungs. Pathogenic bacteria are usually normal anaerobic flora of the oropharyngeal cavity (classically Fusobacterium necrophorum). Initial antibiotic recommendations include ampicillin-sulbactam, piperacillin-tazobactam, or a carbapenem.3 If associated with an internal jugular catheter, it is recommended to add vancomycin as well (in addition to catheter removal).5 The role of anti-coagulation is controversial, and is often reserved for cases of persistent bacteremia, limited response to antibiotics or surgical drainage, or large clot burden.3 In severely refractory cases, surgical exploration of the internal jugular may be warranted.2
Case Conclusion
The patient in this case was taken to the operating room for surgical exploration of his oral cavity with drainage of multiple complex loculated abscesses. He was continued on ampicillin-sulbactam postoperatively and remained hemodynamically stable. He did not receive anticoagulation. He was discharged home on ampicillin-clavulanic acid in stable condition with plans for close follow-up.
References
1. Lemierre A. On Certain Septicaemia Due to Anaerobic Organisms. Lancet. 1936;2:701-703.
2. Riordan T, Wilson M. Lemierre's syndrome: more than a historical curiosa. Postgrad Med J. 2004;80(944):328-334.
3. Golpe R, Marín B, Alonso M. Lemierre's syndrome (necrobacillosis). Postgrad Med J. 1999;75(881):141-144.
4. Chirinos JA, Lichtstein DM, Garcia J, Tamariz LJ. The evolution of Lemierre syndrome: report of 2 cases and review of the literature. Medicine (Baltimore). 2002;81(6):458-465.
5. Andes DR, Urban AW, Acher CW, Maki DG. Septic thrombosis of the basilic, axillary, and subclavian veins caused by a peripherally inserted central venous catheter. Am J Med. 1998;105(5):446-450.



