If a patient presents with recent trauma, neck pain, headache or neck manipulation with signs or symptoms of stroke, cervical artery dissection should be considered.
Case Report
A 28-year-old white male with no significant past medical history presented to the emergency department complaining of dizziness, nausea, and vomiting. He also related a headache and unsteadiness when trying to walk. His significant other noted that he had some slurred speech and right eye deviation as well. He awoke around 5:50 AM feeling normal, fell back asleep, and woke again at 7:00 AM with his presenting constellation of symptoms. He started a construction job about 1 month ago and noted a severe headache while using a jackhammer two days prior to presenting to the ED. Review of systems was otherwise negative. He denied any previous strokes or history of hyperlipidemia or clotting disorders. He had no family history of stroke. He denied alcohol or drug use but noted that he vaped for the past couple years.
On exam, the patient was afebrile, with a heart rate of 98, a blood pressure of 138/74, a respiratory rate of 18, and a pulse oximetry of 100% on room air. He weighed 150 lbs. He appeared anxious and was shaking in bed, but did not have a tremor. Cardiovascular and respiratory findings were unremarkable. He exhibited mild dysarthria, intermittent ophthalmoplegia to both the right and left eyes, and an ataxic gait. No other acute findings were present on physical exam.
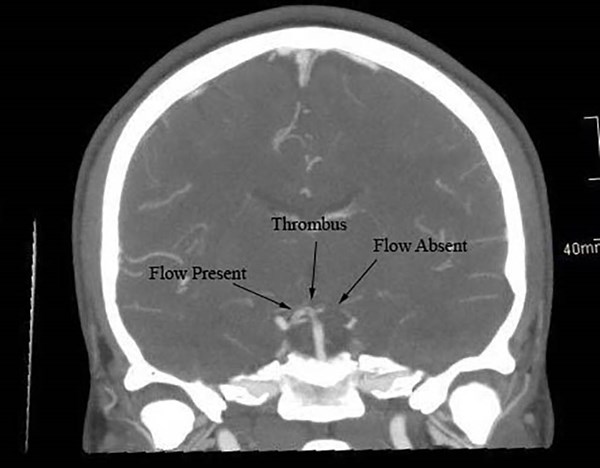
Given the history and physical examination findings, a Code Stroke was activated. The patient’s NIH stroke scale was 3 due to his gaze, dysarthria, and ataxia. A blood glucose level was 164 and his complete blood count and metabolic panel were unremarkable. A CT head without contrast showed a questionable hyperdensity in the distal basilar artery with no acute intracranial hemorrhage or large vessel territory ischemic changes. CT angiogram of the neck showed a luminal irregularity and narrowing of the V3 segment of the left vertebral artery with a nonocclusive thrombus at the C1-C2 level (Figure 1).
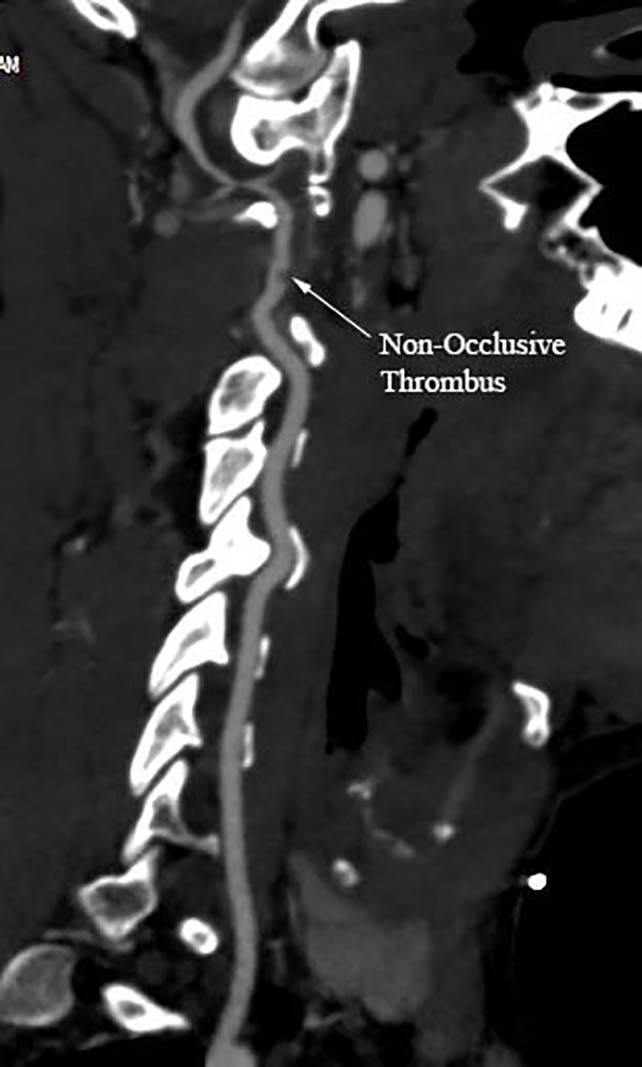
Figure 1. CT angiogram of the neck
These findings were concerning for a vertebral artery dissection. Additionally, CT angiogram of the head showed partial thrombosis of the distal basilar artery and an occlusive thrombus extending into the left superior cerebellar artery (Figure 2).
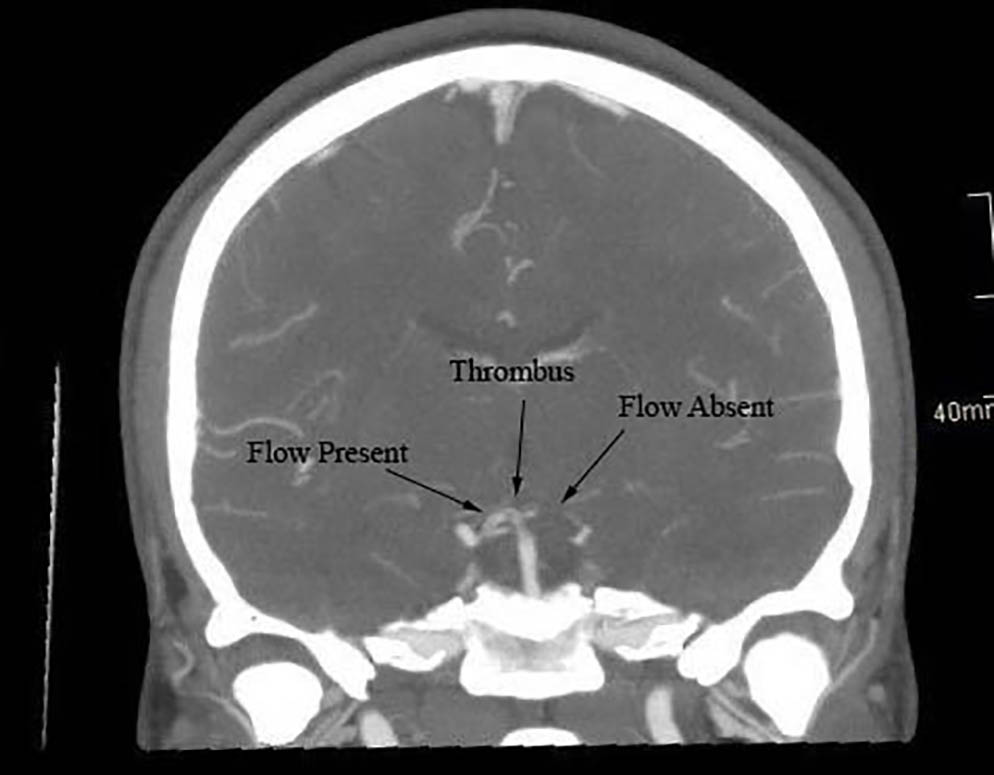
Figure 2. CT angiogram of the head
Due to the two-day duration of the problem, the patient was not a candidate for tPA. The neuro-interventional team assessed the patient and quickly performed an emergent thrombectomy which resulted in successful recanalization of his basilar artery occlusion and TICI 3 flow.
Following his intervention, he was admitted to the neurology intensive care unit for close monitoring of his neurologic status per the unit protocol. Dual antiplatelet therapy was initiated using aspirin (325 mg) and clopidogrel (75 mg) daily. Atorvastatin (80 mg) daily was also added to his regimen. His symptoms resolved and his NIH stroke scale returned to zero at the time of discharge. He received physical and occupational therapy prior to discharge, and was discharged home with no residual deficits.
Our standard stroke workup, including bilateral lower extremity doppler studies, hypercoagulability panel, and echocardiogram was performed in order to expose factors contributing to his stroke. The workup was unrevealing with the exception of a patent foramen ovale with left to right shift.
Discussion
The vertebrobasilar arterial system originates from the subclavian arteries. Infarction of this system results in a posterior circulation stroke. While posterior stroke presentation is not always classic, the most common clinical manifestations include vertigo, loss of balance, diplopia, headache, nausea, slurred speech, limb weakness, and altered consciousness. Dysphagia and Horner’s syndrome may be seen with proximal lesions. On physical exam, patients may display limb weakness, gait ataxia, nystagmus, and unilateral limb weakness. Some causes of posterior circulation stroke include atherosclerosis, embolism and arterial dissection. Atherosclerosis accounts for 35% of posterior circulation strokes, while embolism accounts about 25% and cervical artery dissections about 15%. Given the etiologies of acute posterior circulation infarct MRI is generally the most useful imaging technique; however, CT imaging is more commonly used as the initial imaging modality in patients with symptoms of stroke. As seen in our case report, CT angiogram of the head and neck frequently augment the workup to elucidate vascular abnormalities. The first-line treatment is IV recombinant tissue-plasminogen activator if the patient presents within 4.5 hours of when the patient was last known well. In order to prevent recurrent strokes, risk factors such as hypertension, hypercholesterolemia and clotting disorders must be evaluated and managed.
If a patient presents with recent trauma, neck pain, headache or neck manipulation with signs or symptoms of stroke, cervical artery dissection should be considered. While use of heavy machinery seems to be a rare cause of cervical artery dissection such as in this case, we did find one other reported case of a 48-year-old male who suffered a carotid artery dissection while using a jackhammer. Cervical artery dissections may result from cervical trauma or occur spontaneously and account for the cause of about 15% of strokes in young adults. The vertebral artery segments most commonly involved in dissections are V2 and V3, which course through the transverse foramina and then exit the foramen transversarium of C2 before entering the skull.
Conclusion
One less common cause of posterior circulation strokes is cervical artery dissection. In this case report, a young male patient suffered a posterior circulation stroke due to a vertebral artery dissection. The patient had suffered a severe headache two days prior to presentation while using a jackhammer, and this was presumed to have contributed to his dissection and stroke presentation. In young patients presenting with stroke, a thorough history including occupational history and recent trauma should be done to ensure proper diagnosis and treatment.
References
1. Vadikolias K, Heliopoulos J, Serdari A, Vadikolia CM, Piperidou C. Flapping of the dissected intima in a case of traumatic carotid artery dissection in a jackhammer worker. J Clin Ultrasound. 2009;37(4): 221-222.
2. Nouh A, Remke J, Ruland S. Ischemic posterior circulation stroke: a review of anatomy, clinical presentations, diagnosis, and current management. Front Neurol. 2014;5:30.