Free Fluid on FAST Exam in Patient with Abdominal Pain and Hematuria
Case
A 29-year-old healthy male presented to the ED with a chief complaint of abdominal pain and blood in his urine. The patient was given an emergency severity index (ESI) of three and was placed in a hallway bed. On history, the patient stated that yesterday after dinner, he developed mild, cramping upper abdominal pain that subsided without intervention. The next day, his abdominal pain had spread and was now diffuse and severe in character. He stated that he went to the bathroom early that morning and urine was grossly bloody. He stated, “Now I can’t pee.”
The patient reported he had no abdominal trauma and no medical or surgical history, although he did report a family history of nephrolithiasis. He was afebrile, tachycardic in the 110s, with mildly elevated blood pressure. He appeared uncomfortable. Physical examination revealed a tender abdomen with diffuse, involuntary guarding. Genitourinary exam was unremarkable, and there was no blood at the urethral meatus.
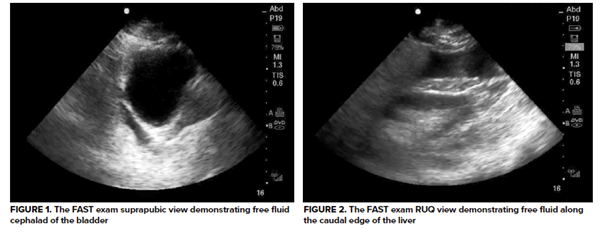
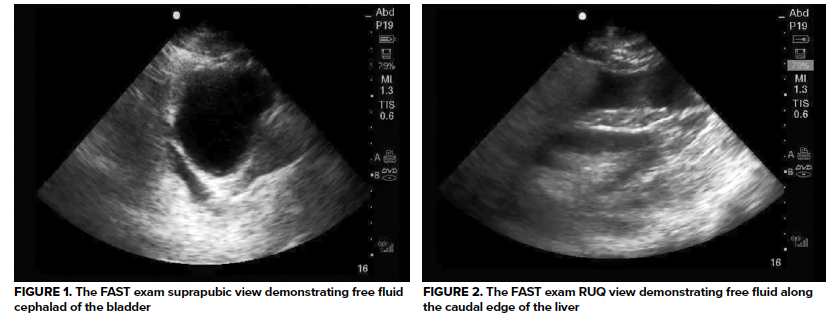
An immediate focused assessment with sonography for trauma (FAST) exam was performed and revealed some surprising findings: anechoic fluid cephalad to a full bladder (see image 1). A right upper quadrant view was obtained, and free fluid was seen at the caudal liver edge in the superior paracolic gutter (see image 2). No free fluid was readily identified on the left upper quadrant view. For completeness, a subxiphoid view was obtained and was negative for pericardial effusion.
A Surprising Twist
At that time, the patient endorsed that he had previously withheld information out of embarrassment. He and his roommate were wrestling the previous night when his roommate tackled him, hitting him in the abdomen. He experienced immediate cramping pain, but because it resolved spontaneously, he did not seek medical attention. When symptoms returned and had worsened the next day, he presented to the ED.
The patient was provided with IV analgesia and fluids. Given his mild tachycardia but otherwise hemodynamic stability, he was taken for a stat CT scan. The scan read: “Mild to moderate ascites. Otherwise, normal CT scan of the abdomen and pelvis.” Bloodwork was still pending, but the patient remained tachycardic despite analgesia and fluid resuscitation. At that time, surgery was consulted for peritonitis and positive FAST exam. After evaluation by surgery, the patient was brought to the operating room where the report read: “4 cm vertical bladder rupture at the dome of the bladder with moderate clear fluid in the abdominal cavity.”
Discussion
Bladder rupture is a relatively rare condition due to the protection of the bladder in the bony pelvis. The most common cause of bladder rupture is blunt force trauma.1,2 Motor vehicle accidents account for most cases; however, iatrogenic injuries associated with surgical or endoscopic procedures have also been described.2,3 Spontaneous bladder rupture is associated with a high risk of mortality. Most patients with bladder rupture have gross hematuria and complain of pelvic pain with difficulty voiding. In stable patients, the gold standard for diagnosis is a retrograde cystogram.1
Bladder rupture is classified as extraperitoneal or intraperitoneal.1-3 Most cases of bladder rupture are extraperitoneal. Extraperitoneal bladder ruptures are often associated with pelvic fractures and occur in deceleration injuries.1 Pelvic fractures should therefore raise suspicion for bladder injury. If the bladder rupture is below the peritoneal reflection (an anatomical landmark separating the intra- and extraperitoneal portions of the rectum), urine extravasation will be extraperitoneal and confined around the bladder. Therefore, FAST examination will not be positive in isolated extraperitoneal bladder ruptures.1,2
Intraperitoneal bladder rupture occurs when compressive forces act against a full bladder.1-3 This can occur in motor vehicle collisions when a full bladder is compressed by the steering wheel or other forces. If the bladder rupture is on the bladder dome and above the peritoneal reflection, urine extravasation will be intraperitoneal. Therefore, FAST examination may be positive in intraperitoneal bladder ruptures as urine enters the abdominal cavity.1,2
Management
Extraperitoneal bladder rupture is typically managed conservatively, as the bladder often heals spontaneously with urinary catheter drainage.1,2 A Foley catheter is placed and remains for a minimum of 10-14 days. On follow-up with urology, a repeat cystogram is performed to confirm healing of the bladder, and the Foley can then be removed.2
According to the American Urological Association guidelines, intraperitoneal bladder ruptures should be surgically repaired.2 This is because intraperitoneal ruptures are associated with an increased risk of larger lacerations that rarely heal with the placement of urinary catheter drainage alone.
Additionally, untreated intraperitoneal bladder ruptures can lead to peritonitis and electrolyte derangement as urine is resorbed. It can also lead to intraabdominal infection, sepsis, and renal failure. Following operative repair, a Foley catheter is placed for 10-14 days. A follow-up cystogram is then performed to confirm healing of the bladder, and the Foley can then be removed.
Case Conclusion
Urology was consulted intraoperatively by general surgery after no further traumatic injuries were identified. Urine had already been evacuated from the abdominal cavity and the patient had a Foley in place. Following its closure, the bladder was filled through the Foley catheter with approximately 300 mL of normal saline with no leakage identified. A pelvic drain was placed.
The patient was already in the operating room when his blood work resulted. His pre-operative creatinine was 2.30, nearly triple his baseline. The patient remained on the general surgery service. On hospital day two, he regained bowel function and tolerated a soft diet. His creatinine normalized by hospital day four. He was discharged after six days in the hospital. He followed up with urology 14 days later. Repeat cystogram revealed no evidence of residual bladder leak. The Foley catheter was removed, and the patient was able to spontaneously void. He reported no further complaints on further follow-up notes.
Take-Home Points
- In a patient with signs of peritonitis on clinical exam, FAST examination may help identify those who need early operative intervention.
- Be wary of CT reads that do not fit the clinical picture. In a completely healthy 29-year-old, findings such as “moderate ascites” on a CT should prompt further investigation.
- Although rare, intraperitoneal bladder rupture must remain on the differential in blunt abdominal trauma. This injury is managed operatively due to risk of electrolyte derangements, sepsis, and renal failure as urine is resorbed into systemic circulation.
References
- Radswiki. Urinary bladder rupture: Radiology reference article. Radiopaedia Blog RSS. Accessed August 1, 2021.
- Simon LV. Bladder rupture. StatPearls [Internet]. Published May 27, 2021. Accessed August 3, 2021.
- Voelzke. Traumatic and iatrogenic bladder injury. UpToDate. www.uptodate.com. Accessed August 1, 2021.