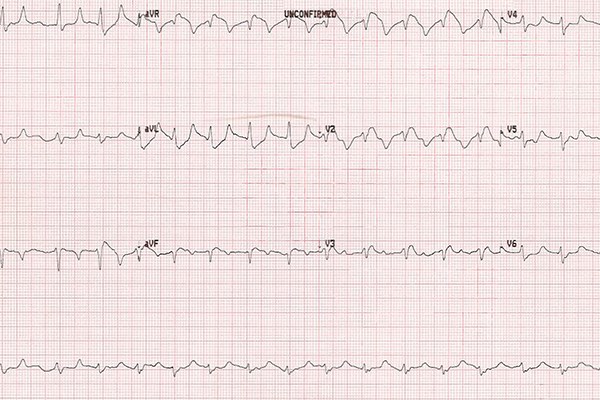
A 60-year-old female presents to the ED with worsening generalized weakness and SOB over the past 3 days. Her history is significant for ESRD and she missed dialysis today. Initial vital signs were grossly unremarkable. An EKG obtained at triage (Figure 1) showed sinus rhythm with first degree AV block and peaked T-waves.
Figure 1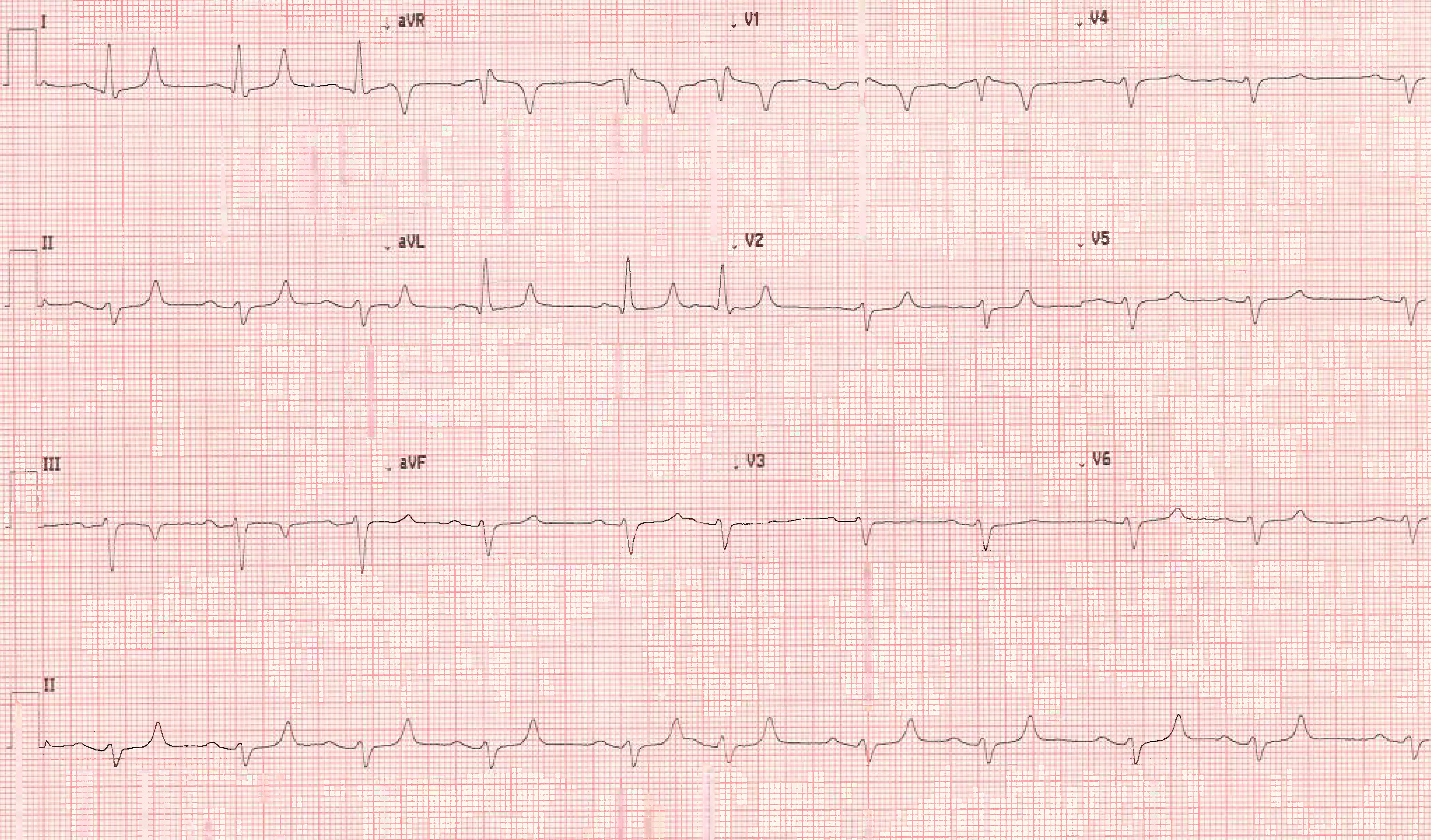
The patient was brought to a room and placed on the monitor, which showed a wide complex tachycardia. A repeat EKG (Figure 2) showed a widening QRS, loss of P-waves, and ST-segment changes all concerning for an impending sinoventricular rhythm. Labs sent from triage showed a hyperkalemia of 8.8 mEq/L.
Figure 2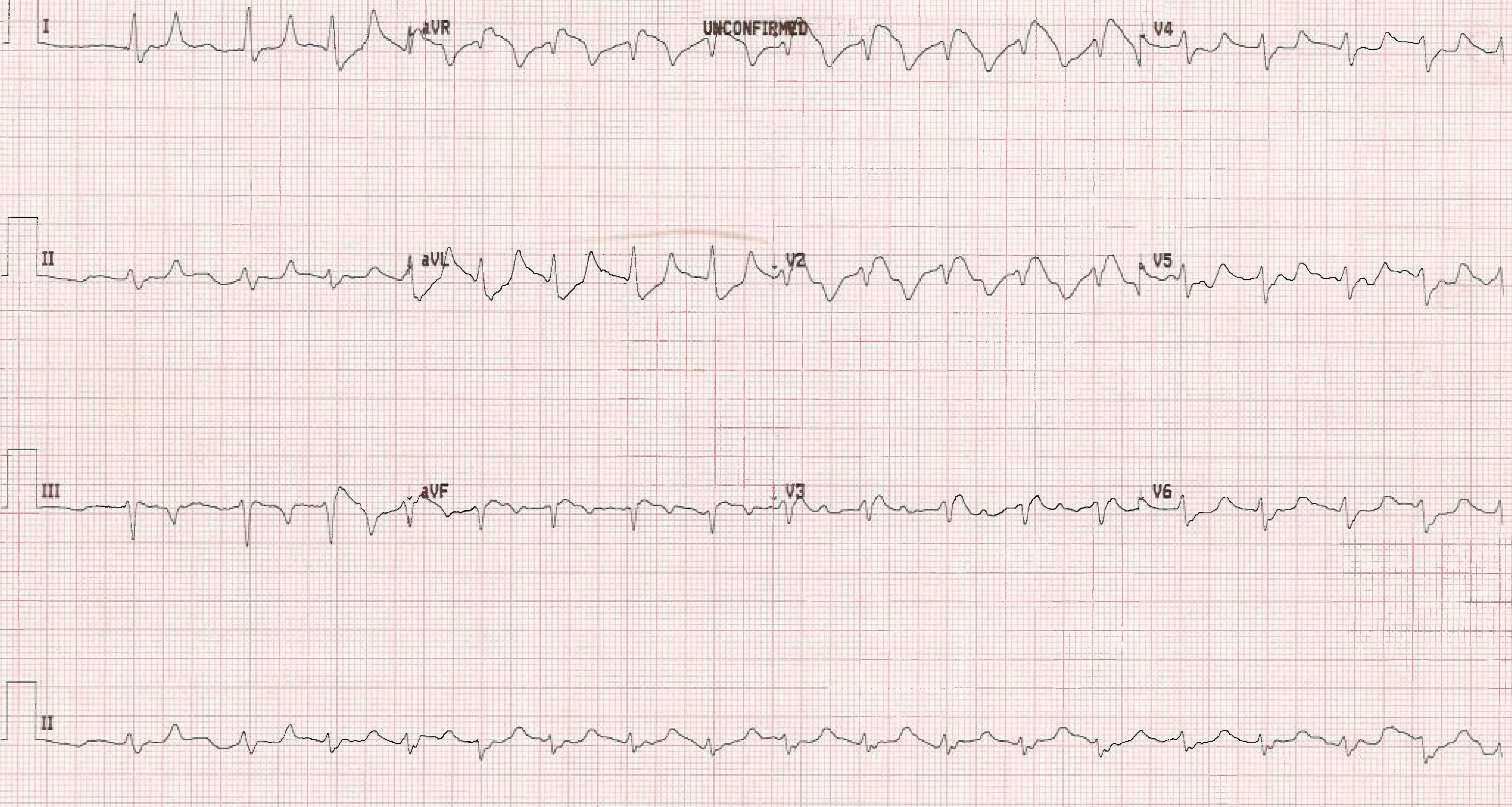
Introduction
Hyperkalemia is generally defined as a potassium level > 5.5 mEq/L and can be further classified as mild (5.6–6.0 mEq/L), moderate (6.1–7.0 mEq/L), and severe (> 7.0 mEq/L). Etiologies frequently seen in the ED include renal failure, hemolysis, rhabdomyolysis, adrenal insufficiency, acidosis, and medication effects (eg, ACE-I, ARB, B-Blockers).
The cardiac manifestations of hyperkalemia stem from its effect on the resting membrane potential. Elevated plasma potassium concentrations reduce this potential, leading to a decreased influx of sodium. The net result is an action potential with reduced amplitude and slower conduction. As the conduction delays worsen (reflected on the ECG by widening of the QRS complex), the risk of ventricular dysrhythmias, including ventricular fibrillation, increases. Severe hyperkalemia can alter the resting membrane potential sufficiently to reduce automaticity of cardiac pacemaker cells, leading to severe bradycardia or even asystole.1
EKG Changes
The EKG changes seen in hyperkalemia are typically sequential and correlate with the severity of hyperkalemia. While often seen in the following order, there are exceptions to the rule, and changes can be rapid and easily missed.
- Peaked, symmetric T-waves with a narrow base
- PR prolongation and QT shortening
- QRS widening and decreased P-wave amplitude
- Increased QRS widening (both initial and terminal portions) and loss of P-waves
- Sine-wave pattern (sinoventricular rhythm)
- VF, asystole2
A helpful tip to remember the EKG changes that follow peaked T-waves is to imagine the PQRS-T complex being pulled from either side like a string.
It is important to reinforce that an EKG is specific but not sensitive for hyperkalemia as patients can have only minimal EKG changes despite high potassium levels. As well, the EKG changes may not always be sequential, and a life-threatening dysrhythmia can occur at any time at almost any potassium level.
Treatment
The goals of treatment are stabilizing the resting membrane potential, shifting potassium intracellularly, and eliminating potassium from the body. A helpful pneumonic is "C B2IG K Drop."
Calcium
This can either be calcium gluconate via a peripheral line or calcium chloride if central access is available. Calcium chloride contains more calcium per mL but extravasations can lead to tissue necrosis. Calcium counteracts potassium's depolarizing effects, stabilizing the cardiac membrane and decreasing the risk for dysrhythmias.
Dose: 10 mL of 10% solution over 2-5 minutes, repeat every 5 minutes until EKG normalizes
Onset of action: < 3 min
Duration: ~20-50 min
Beta-agonist
This is typically nebulized albuterol which is readily available and can be administered without IV access. It works by shifting potassium from the serum into the cells. The efficacy of albuterol maybe increased when used in combination with insulin and dextrose.
Dose: 10-20 mg nebulized over 10 min
Onset of action: 15-30 min
Duration: 2-4 hrs
Bicarbonate
While traditionally considered part of the hyperkalemia treatment "cocktail," the literature doesn't support its use with hyperkalemia in the setting of a normal pH. Bicarbonate infusions (not boluses) may play a role in the treatment of patients who are both acidotic and hyperkalemic.
Insulin and Glucose
This should be the first IV treatment given after calcium. It works by shifting potassium into the cells. The effect is dose dependent and the dose of glucose should be adjusted per the patient's blood glucose level and risk factors for hypoglycemia (renal disease, use of diabetic medications, etc.).
Dose: 10 units regular insulin IV with 25-50 grams (1-2 amps) 50% dextrose solution
Onset of action: 10-30 min
Duration: 2-6 hrs
K represents Kayexalate (sodium polystyrene sulfonate)
SPS is a cation exchange resin that binds potassium in the gut and increases fecal potassium excretion. Because of questionable safety and efficacy, its role in the treatment of hyperkalemia is limited. Patiromer sorbitex calcium is a new cation exchange polymer approved for hyperkalemia. Neither of these medications are indicated for acutely treating hyperkalemia.
Dialysis (and Diuretics)
Dialysis is the most effective and reliable treatment to remove potassium. While bedside dialysis can sometimes be arranged fairly quickly (depending on your ED setting), patients will often require the other treatments as temporizing measures given the acuity of their presentation.
Diuretics can also be considered in patients who still make urine. Loop diuretics, such as furosemide, lead to the most potassium excretion.
Case Continued
The patient was given calcium gluconate, nebulized albuterol, and insulin with dextrose. A few minutes after the calcium was administered, a repeat EKG (Figure 3) showed improvement of the QRS duration and ST-segment abnormalities.
Figure 3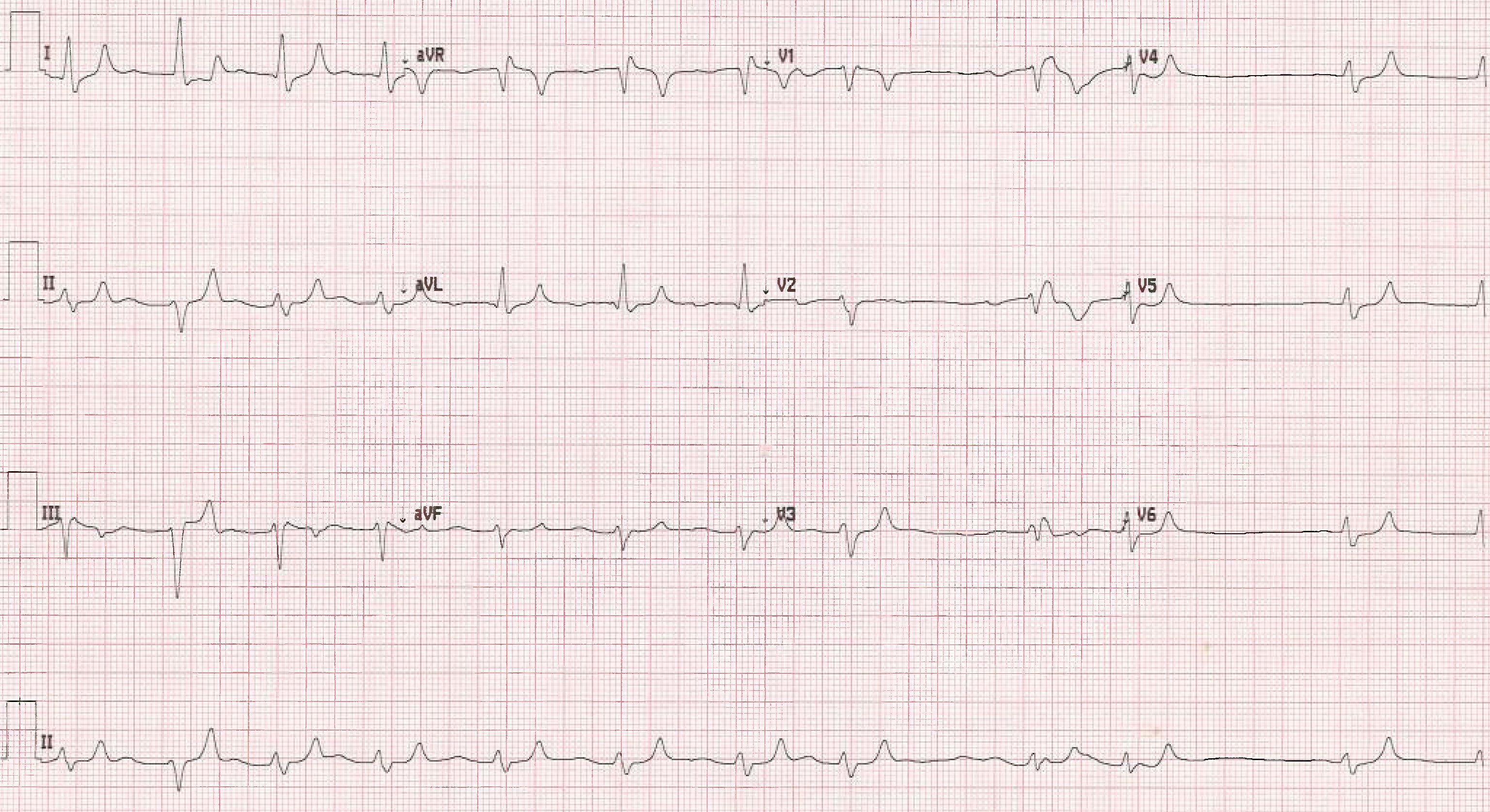
While arranging for emergent dialysis, the patient was noted to be in a WCT on the monitor. A repeat EKG (Figure 4) showed a regular WCT.
Figure 4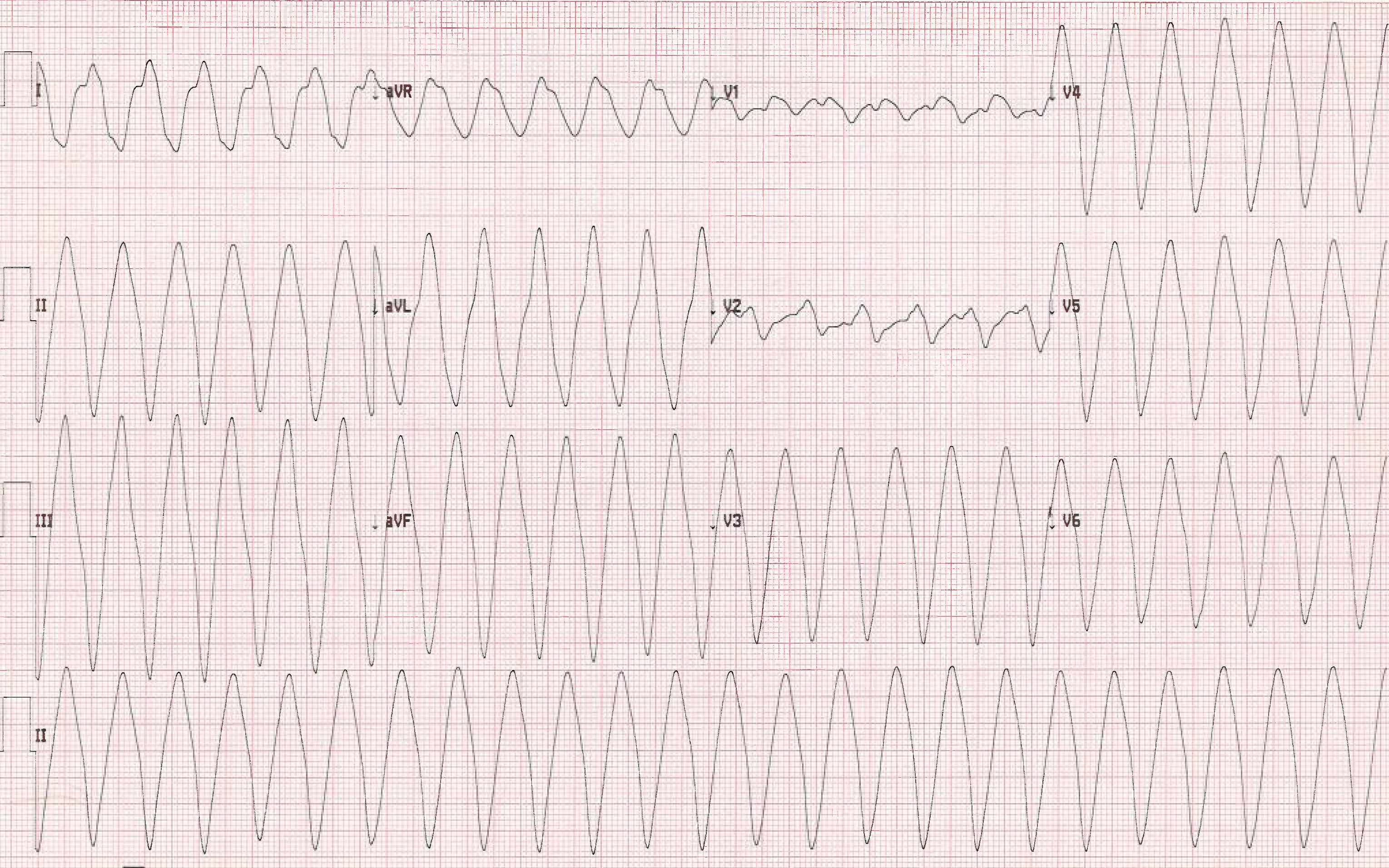
The patient remained hemodynamically stable, and while discussing treatment options, amiodarone was considered and discarded as a treatment option – but why?
Further Treatment
Amal Mattu, MD, FACEP, describes hyperkalemia as sodium channel "poison." Administering a sodium blocking antidysrhythmic medication to treat a WCT in the setting of hyperkalemia would exacerbate this problem, leading to what he calls a "clean kill." (Note: Search "clean kill wide complex tachycardia" on the Essentials of Emergency Medicine channel on YouTube for Dr. Mattu's lecture on "regular really wide complex tachycardia.")
Cardioversion is the safest treatment for patients with an unstable WCT and hyperkalemia. This needs to be done in conjunction with aggressive treatment of the hyperkalemia, most importantly membrane stabilization, to prevent further episodes of dysrhythmias. Magnesium can be considered if the patient is known to have hypomagnesemia, but otherwise does not play a role in the treatment of hyperkalemia or its associated dysrhythmias.
Case Resolution
The WCT resolved spontaneously, and dialysis was emergently started in the ED. The patient was admitted and was discharged home after an uneventful hospital course.
References
1. Redfors B, Dordi R, Ben-Yehuda O. The Kidney in Heart Disease. In: Fuster V, Harrington RA, Narula J, Eapen ZJ. eds. Hurst's The Heart, 14e New York, NY: McGraw-Hill. Accessed March 28, 2018.
2. Ritchie JV, Juliano ML, Thurman R. ECG Abnormalities. In: Knoop KJ, Stack LB, Storrow AB, Thurman R. eds. The Atlas of Emergency Medicine, 4e New York, NY: McGraw-Hill. Accessed March 28, 2018.
3. Weisberg LS. Management of Severe Hyperkalemia. Crit Care Med. 2008;36(12):3245-3251.