Hemoperitoneum during pregnancy is an emergent condition that places the mother and fetus at risk.
In a woman of childbearing age, the most common sources of hemoperitoneum are ectopic pregnancy and ruptured ovarian cysts.1 The corpus luteum is a functional cyst that develops from an ovarian follicle during the luteal phase of each menstrual cycle. If a vessel supplying the corpus luteum ruptures, the patient may hemorrhage with blood spilling into the peritoneal cavity resulting in hemoperitoneum. We present the case of hemoperitoneum in a pregnant woman resulting from a hemorrhagic corpus luteum during her first trimester of pregnancy.
Case
A 25-year-old G4P3003 female presented to the emergency department (ED) with a chief concern of abdominal pain and emesis since the prior evening. The patient was brought immediately to the ED resuscitation room upon arrival due to the severity of her abdominal pain as well as her vital signs. Her vitals were: BP 87/64 mmHg; HR 118; Resp 20, SpO2 100%, Temp measured 96.8 °F, BMI 23.7 kg/m2. The patient’s pain had started the night before while she was laying down. She described it as severe (10/10), localized to the right upper quadrant, and with radiation to her shoulder. She had unrelenting nausea and vomited multiple times. She also had multiple episodes of non-bloody diarrhea. Her last menstrual period was 27 days prior to presentation, and she did not think she was pregnant. ROS was unremarkable. Of note, the patient’s past surgical history included the removal of an intrauterine device due to displacement a couple of months ago.
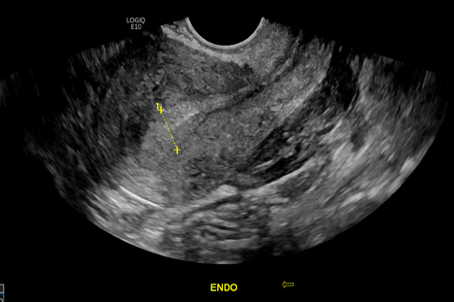
In the trauma room, large-bore intravenous access was obtained and resuscitation was started with 1L NS. A bedside RUSH exam was performed, noting free fluid in Morrison's pouch and in the splenorenal space. Laboratory findings were significant for: leukocytes 20.9 x10^3 /mcL, hemoglobin 10.4 gm/dL, lactic acid 4.3 mmol/L, and a beta hCG quant 18 mIU/mL (which corresponded to an indeterminate result per the lab’s reference range). The formal abdominal ultrasound showed complex free fluid suspicious for hemoperitoneum and was otherwise unremarkable (FIGURE 1), and transvaginal ultrasound showed a structure of complex echogenicity in the right adnexa, which included a small cystic region with a surrounding thick rim, of approximately 5.9 x 7.9 x 7.7 cm.

These findings were suspicions for right-sided ectopic pregnancy without an intrauterine gestation. (FIGURE 2)
The patient was taken emergently to the operating room for diagnostic laparoscopic surgery with OB where 1500 mL of blood was evacuated and a ruptured hemorrhagic cyst ligated. The patient was discharged on post-operative day 2 after receiving one unit of RBCs and having a doubling of her beta-hCG, which provided reassurance of possible fetal viability.
Discussion
Hemoperitoneum due to a ruptured corpus luteum in early pregnancy is a rare occurrence2. The corpus luteum is a functional cyst that develops from an ovarian follicle during the luteal phase of each menstrual cycle. The area forms a dense network of capillary vessels that enable the production of progesterone needed to maintain early pregnancy until the placenta produces its own progesterone around week eight2. Normally, if conception does not occur, the corpus luteum goes through apoptosis around the time of menstruation. If the corpus luteum remains, it can fill with fluid or blood thereby forming a cyst.
During early pregnancy, there is a substantial increase in the stability of the vessels that supply blood to the corpus luteum3. When one of those vessels supplying the corpus luteum ruptures, the patient hemorrhages into the peritoneum. Spontaneous hemoperitoneum can be a gynecological emergency, thus it is important to diagnose early and consult the gynecology service.
In the presented case, performing a bedside FAST exam was very beneficial because it immediately showed the presence of fluid in the abdominal cavity.
Conclusion
In summary, the corpus luteum is a functional cyst that produces progesterone during early pregnancy. In rare occasions, the corpus luteum can rupture and result in hemoperitoneum and hemodynamic instability. The use of bedside RUSH exam can be used to visualize peritoneal or pelvic fluid in an unstable patient and thereby reduce the time from arrival to treatment.
References
- Meghan Lubner, Christine Menias, Creed Rucker, Sanjeev Bhalla, Christine M. Peterson, Lisa Wang, Brett Gratz. Blood in the Belly: CT Findings of Hemoperitoneum. Radiographics Vol 27 No 1 Jan 1 2007
- Bauman R, Horvat G. MANAGEMENT OF RUPTURED CORPUS LUTEUM WITH HEMOPERITONEUM IN EARLY PREGNANCY - A CASE REPORT. Acta Clin Croat. 2018;57(4):785-788. doi:10.20471/acc.2018.57.04.24
- Fraser HM, Wulff C. Angiogenesis in the corpus luteum. Reprod Biol Endocrinol. 2003;1:88. Published 2003 Nov 10. doi:10.1186/1477-7827-1-88
- Fiaschetti V, Ricci A, Scarano AL, et al. Hemoperitoneum from corpus luteal cyst rupture: a practical approach in emergency room. Case Rep Emerg Med. 2014;2014:252657. doi:10.1155/2014/252657
- N. Gupta, V. Dadhwal, D. Deka, S. K. Jain, and S. Mittal, “Corpus luteum hemorrhage: rare complication of congenital and acquired coagulation abnormalities,” The Journal of Obstetrics and Gynaecology Research, vol. 33, no. 3, pp. 376–380, 2007.



