This case study highlights the need to investigate patients who present with non-specific complaints with a potentially life-threatening cause in mind.
Editor’s note: This article is adapted from the author’s poster presentation at EMRA Case-Con 2018.
Fatigue and generalized weakness are commonly encountered complaints in the emergency department.1 The workup of these patients is often challenging because of the broad range of possible etiologies. Fatigue and generalized weakness are hence classified as “non-specific symptoms” since the differentials range over 14 ICD-10 categories.2 Amidst the patients who present to the ED with nonspecific complaints, 60% tend to have a serious outcome within the next 30 days3 and have significantly higher mortality than the patients who present with specific complaints.4 ED guidelines on the approach to patients who present with nonspecific complaints are not very well established. In 56% of patients who present to the ED with nonspecific complaints, the primary ED diagnosis did not correlate with the discharge diagnosis.5
This case report describes the case of a 56-year-old woman with a medical history significant for Type 2 diabetes, hyperlipidemia, hypertension, and linear IgA bullous dermatosis, who presented with a 6-day history of fatigue and generalized weakness. Upon investigation, this fatigue was attributed to drug-induced hemolysis, with an underlying drug interaction between dapsone and hydrochlorothiazide potentiating the adverse effect. This case study highlights the need to investigate patients who present with non-specific complaints with a potentially life-threatening cause in mind.
Case Presentation
A 56-year-old female presented to the ED complaining of worsening fatigue and weakness for 6 days. She denied any flank pain, fevers, runny nose, chills, headaches, abdominal pain, changes in bowel movements, melena, or urinary complaints such as hematuria or dysuria. There was no history of recent travel, exposure to sick contacts, or trauma.
Her past medical history was significant for Type 2 diabetes, hyperlipidemia, hypertension, and linear IgA bullous dermatosis. The patient was previously on lisinopril for hypertension, however 3 months prior the patient started to notice a diffuse rash with vesicles on her body for which she consulted a dermatologist. She was deemed to have an allergy to lisinopril, which was discontinued. She was started on prednisone of an unrecalled dose, which was subsequently stopped when the rash subsided. However, the rash came back a few weeks later, and a biopsy confirmed the diagnosis of linear IgA bullous dermatosis. The patient was started on dapsone 25 mg QD, and her G6PD workup was negative. She has been following up with her dermatologist for weekly blood counts.
One week prior to the ED visit, the patient's dapsone dose was increased to 100 mg QD, her hemoglobin was documented at 11.4 g/dL, and she was started on hydrochlorothiazide for hypertension.
Physical examination showed a pale-appearing female. Vital signs were stable except for an elevated blood pressure of 145/77 mmHg. She had significant conjunctival pallor and icterus without any edema. The rest of the physical examination findings were within normal limits.
Fingerstick glucose on admission to the ED was 458 mg/dL without an elevated anion gap or beta-hydroxybutyrate. She was started on 1 L of normal saline over 1 hour and was given 8 units of insulin. Repeat blood glucose level after 90 minutes was 167 mg/dL. Blood was obtained and showed a complete blood count remarkable for anemia at 7.2 g/dL with reticulocytosis. Total bilirubin levels were elevated at 4.2 mg/dL with predominantly unconjugated hyperbilirubinemia. Elevated LDH levels of 773 U/L was present. Urine analysis showed a moderate hematuria and the presence of urobilinogen. The fecal occult blood test was negative. Chest X-ray was normal and CT abdomen didn’t show any bleeding. Two units of packed cells were transfused while in the ED.
The patient was diagnosed with hemolytic anemia, which was thought to be precipitated by dapsone and hydrochlorothiazide. The offending medications were stopped, and the patient was admitted to the medical service. Hemoglobin level gradually improved, and the patient reported clinical improvement on discharge.
Discussion
This is a case of a middle-aged female who presented with complaints of generalized weakness and fatigue. There are no established guidelines on how to approach a patient presenting with non-specific complaints such as fatigue. Infectious, metabolic, and oncologic processes – many with poor outcomes – are often associated with this presentation.6 Because of this, we recommend a wide diagnostic approach in these patients. Obtaining a detailed history, specifically looking for inciting events that precipitated the condition, can provide useful diagnostic clues. A detailed review of the patient’s medications is essential for a complete history.
Elderly patients who visit the ED are taking an average of 4.2 different kinds of medications per day, and adverse drug reactions contribute to 10.6% of their ED visits.7 A detailed physical examination can often unmask important clues to the diagnosis. Neurological causes of weakness have to be evaluated quickly since the management of these conditions is often time sensitive. In this patient, the review of medications revealed that the patient was prescribed dapsone and hydrochlorothiazide, and physical examination showed the presence of anemia.
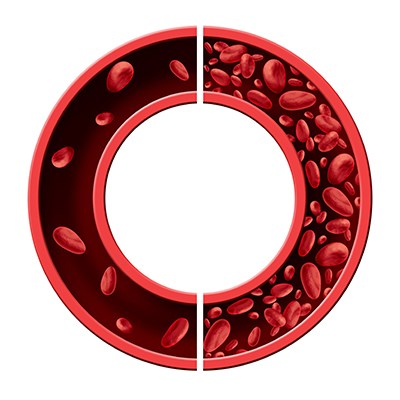
The primary step in the approach to any patient presenting with anemia is to determine whether it is acute or chronic.8 Our patient had a 4 mg/dL reduction in her hemoglobin levels over a period of 1 week, which was highly concerning for acute blood loss. Blood loss is the most common cause of clinically significant anemia;9 however, the patient didn’t report any hematemesis, melena, hematochezia, hematuria, vaginal bleeding, or any cutaneous bleeding episodes. The stool was negative for the presence of occult blood. She had elevated reticulocyte count, serum lactate dehydrogenase levels, and an unconjugated hyperbilirubinemia with preserved RBC morphology, which was suggestive of acute hemolytic anemia. Review of medications revealed her use of dapsone and hydrochlorothiazide which pointed us towards the diagnosis of drug-induced hemolytic anemia as a probable cause of her symptoms. However, confirmation of this is beyond the scope of the ED.
The management of anemia in the ED primarily focuses on determining the immediately correctable causes and determining the need for blood transfusion. The threshold to initiate blood transfusion in individuals with asymptomatic anemia is less clear.8,10 Hemoglobin levels less than 7 g/dL is commonly used as the threshold to initiate blood transfusions11 and in patients with an acute drop in hemoglobin levels or in individuals with symptomatic anemia, the clinician can initiate transfusions at much higher levels.12 In a patient who is not actively bleeding, each unit of transfused RBCs increases the hemoglobin levels by about 1g/dL13 and this effect can be observed in patients as early as 15 minutes after the completion of the transfusion.14
Dapsone has long been known to cause hemolytic anemia, especially in people with G6PD deficiency; it causes a drop in hemoglobin levels up to 3 g/dL in up to 16% of the patients who receive a standard dose.15 This effect has been attributed to the generation of free radicals and protein mixed disulfides in red blood cells.16 Dapsone has been recommended for the treatment of leprosy, dermatitis herpetiformis, brown recluse spider bite, and linear IgA bullous dermatosis.17 Testing the patient for G6PD enzyme deficiency has been recommended prior to initiating dapsone, along with periodic monitoring of hemoglobin. levels.17 Hydrochlorothiazide causes anemia by the mechanism of immune hemolytic anemia.18 There haven’t been any reported cases of hemolytic anemia resulting from the combined use of dapsone and hydrochlorothiazide to the author’s knowledge. Since the mechanism of hemolysis is different in both dapsone and hydrochlorothiazide, the combined use of these medications may result in a much higher drop in hemoglobin levels than if they were used alone.
This case emphasizes the need to approach the patients with non-specific complaints presenting to the emergency department with broad and potentially life-threatening outcomes in mind. This is also the first reported case of a combined effect of hemolytic anemia in a patient without G6PD enzyme deficiency taking dapsone and hydrochlorothiazide.