A 79-year-old man with a history of prior bilateral corneal surgeries presented to the ED via EMS for evaluation of eye pain and vision loss.
The patient reported he fell forward from a chair at home, striking the right side of his face against a coffee table, and subsequently experienced complete vision loss in his right eye.
On examination, there was a laceration on the right eye at the temporal edge of the limbus, anisocoria, and right-sided proptosis. Images of the patient at time of initial examination are represented in Images 1a and 1b.

Image 1a: The patient’s right eye, anterior view, upon arrival to the ED

Image 1b: The patient’s right eye, lateral view, upon arrival to the ED
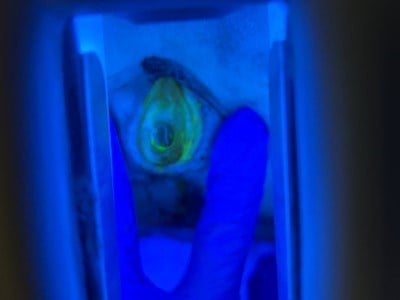
Patient factors including limited mobility prevented the use of a slit lamp to examine the eye. Instead, a Wood’s lamp examination with fluorescein staining was obtained at bedside and a positive Seidel test was observed, as depicted in Images 2a and 2b.
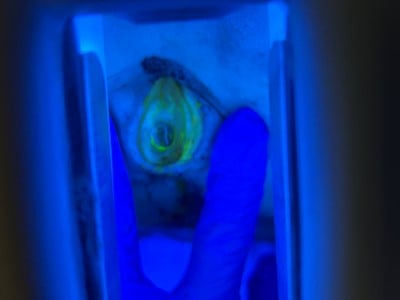
Image 2a: The patient’s right eye, anterior view, under fluorescein staining through Wood’s lamp in the ED
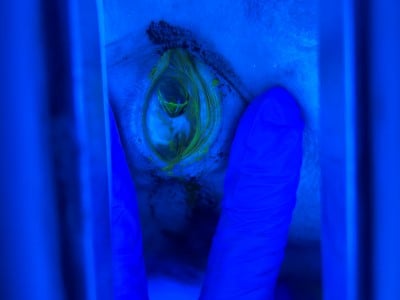
Image 2b: The patient’s right eye, temporal view, under fluorescein staining through Wood’s lamp in the ED
Tonometry was deferred due to our high degree of suspicion for open globe injury (OGI). Differential diagnoses included conjunctival laceration, scleral injury, corneal laceration, OGI, retrobulbar hematoma, and intraocular hematoma.
Computed tomography (CT) of the head and neck was obtained, and key images are shown in Images 3a and 3b. CT showed intraocular hematoma, but no retrobulbar hematoma was identified. No lateral canthotomy was indicated to relieve the proptosis. Additionally, no intracranial or bony calvarial injury was identified, and no other traumatic injuries requiring acute management were discovered. Empiric antibiotic therapy with IV cefazolin and Tdap was initiated. A makeshift eye shield was fashioned from a styrofoam cup, cut to fit the patient’s facial contour, and placed over the affected eye.

Image 3a: Transverse view of the CT non-contrast of the head demonstrating evidence of intraocular hemorrhage of the right eye

Image 3b: Sagittal view of the CT non-contrast of the head demonstrating evidence of intraocular hemorrhage of the right eye
Our facility did not have an on-call ophthalmologist available, and the patient was promptly transferred to a quaternary care center for further management.
Discussion
OGI refers to a full thickness injury of the eye, involving the cornea, sclera, or both.1 The Birmingham Eye Trauma Terminology (BETT) system is used to define types of eye injuries. OGIs are further categorized as a rupture, referring to a full-thickness injury of the eyewall by a blunt object, or a laceration, referring to a full-thickness injury of the eyewall caused by a sharp object due to penetration, perforation, or intraocular foreign body.1
OGIs have the highest incidence among young adult males, usually occurring in those 30-40 years of age.2-7 However, there is also a smaller peak in incidence in the elderly females, especially those 70-89 years of age.2,6,7 The cause of open globe injury varies with age.4-6 In younger age groups, globe laceration is more likely to result from assault, workplace injuries (e.g., working with metal), and motor vehicle accidents.4-6 In older age groups, globe rupture resulting from falls accounted for the majority of injuries.2-7 Of those with falls causing globe rupture, the majority of patients have a history of previous intraocular surgery.2,4,6
OGIs often result in loss of visual acuity. Studies have found globe ruptures to be associated with visual acuity <20/200 in up to 60% of patients.7,8 Globe ruptures can also result in evisceration or enucleation.7 Endophthalmitis is another complication of OGI, which occurs mostly from lacerations rather than ruptures.2,7,9 Primary repair within 24 hours, intraocular tissues prolapse, and self-sealing of wounds were found to decrease the risk of development of endophthalmitis.9 Intravitreal antibiotics and corticosteroids remain controversial for the prophylaxis of endophthalmitis, but vitrectomy is recommended.9
Management
In the ED, there should be a high degree of suspicion for OGI in patients with significant blunt force trauma to the eye, especially in individuals with a history of prior ocular surgery.10 Patients with suspected OGI should have minimal manipulation of the eye during the ocular examination in the ED. Definitive management is surgical intervention. In preparation for surgery, a protective shield should be placed over the affected eye, tetanus status should be updated, and prophylactic antibiotics should be administered with coverage for Staphylcoccus aureus, Bacillus species, and Pseudomonas species. First-line antibiotics are cefazolin 1g IV or vancomycin, plus a 4th-generation fluoroquinolone.
Case Conclusion
Review of external records revealed that after transfer to the receiving facility, the patient was evaluated by the ophthalmology team and promptly taken to the OR. Operative evaluation confirmed there was full thickness globe injury via dehiscence of a former keratoplasty, as well as lens dislocation. The wound was reapproximated, and subconjunctival injections of vancomycin, ceftazidime, and dexamethasone were administered.
The patient was admitted and treated for elevated intraocular pressures with acetazolamide as well as timolol and atropine drops. The patient’s course was complicated by choroidal hemorrhage, for which he underwent a vitrectomy, and then was discharged. At a 2-month follow-up visit, visual acuity in the affected eye without correction was noted to be hand motions.
References
- Kuhn F, Morris R, Witherspoon CD. Birmingham Eye Trauma Terminology (BETT): terminology and classification of mechanical eye injuries. Ophthalmology Clinics of North America. 2002;15(2):139-143. doi:10.1016/S0896-1549(02)00004-4.
- Andreoli MTBA, Andreoli CMMD. Geriatric traumatic open globe injuries. Ophthalmology. 2011;118(1):156-159. doi:10.1016/j.ophtha.2010.04.034.
- Mohseni M, Blair K, Gurnani B, Bragg BN. Blunt eye trauma. In: Aboubakr S, Abu-Ghosh A, Adibi Sedeh P, et al, eds. StatPearls. StatPearls Publishing; 2023. Accessed August 8, 2023. https://www.ncbi.nlm.nih.gov/books/NBK470379/.
- Beshay N, Keay L, Dunn H, Kamalden TA, Hoskin AK, Watson SL. The epidemiology of open globe injuries presenting to a tertiary referral eye hospital in Australia. Injury. 2017;48(7):1348-1354. doi:10.1016/j.injury.2017.04.035.
- Blair K, Alhadi SA, Czyz CN. Globe rupture. In: Aboubakr S, Abu-Ghosh A, Adibi Sedeh P, et al, eds. StatPearls. StatPearls Publishing; 2023. Accessed August 18, 2023. https://www.ncbi.nlm.nih.gov/books/NBK551637/.
- Hughes E, Fahy G. A 24-month review of globe rupture in a tertiary referral hospital. Irish Journal of Medical Science. 2020;189(2):723-726. doi:10.1007/s11845-019-02097-2.
- Coelho J, Ferreira A, Kuhn F, Meireles A. Globe ruptures: outcomes and prognostic analysis of severe ocular trauma. Ophthalmologica. 2022;245(4):376-384. doi:10.1159/000523705.
- Kuhn F, Morris R, Witherspoon CD, Mann L. Epidemiology of blinding trauma in the United States Eye Injury Registry. Ophthalmic Epidemiology. 2006;13(3):209-216. doi:10.1080/09286580600665886.
- Zhang Y, Zhang MN, Jiang CH, Yao Y, Zhang K. Endophthalmitis following open globe injury. British Journal of Ophthalmology. 2010;94(1):111-114. doi:10.1136/bjo.2009.164913.
- Guluma K, Lee J. Ophthalmology. In: Walls R, ed. Rosen’s Emergency Medicine Concepts and Clinical Practice. 10th ed. Elsevier; 2023:750-780.