Only half of all patients who are hemodynamically unstable will respond to a fluid bolus. How can you predict which half your patient falls in?
Only half of patients who are hemodynamically unstable will respond to a fluid bolus.1 There are no historical or physical examination findings that can help us decide whether a patient is a fluid responder, but we must treat hypotension, as we do know that a mean arterial pressure (MAP) less than 60 mmHg increases the risk of death and acute kidney injury (AKI).2,3
Empirical fluid administration is the mainstay of treatment for the hemodynamically unstable patient, but continued fluid resuscitation of the fluid non-responder, or even the fluid responder, can be detrimental. The CLOVERS trial (Crystalloid Liberal or Vasopressors Early Resuscitation in Sepsis) is comparing the restrictive use of fluids and early vasopressors to liberal fluids and rescue vasopressors. This study is expected to be complete in 2021. Given the potential harm from fluid therapy, determining if a patient is on the slope of their Frank-Starling curve will enable to you be far more accurate in determining if your patient is of the 50% who will respond to a fluid bolus.
There are several measures to predict fluid responsiveness. Static measures such as central venous pressure and pulmonary artery occlusion pressure have not been shown to predict fluid responsiveness. Ultrasound measurement of the inferior vena cava (IVC) diameter has not been shown to predict fluid responsiveness. IVC collapsibility index (IVVCI) has conflicting evidence in spontaneously breathing patients, but may be modestly useful if an IVC is very collapsible (> 40%), or very distended (< 15% collapsible).4-6 IVCCI performed better in mechanically ventilated patients,7-9 but similar to the studies in spontaneously breathing patients, they are limited by heterogeneity, small study populations, no standard probe axis, and no standard measurement location.
Dynamic measures of fluid responsiveness perform better than static measures. These include pulse pressure variation (PPV), stroke volume variation (SVV), pulse contour analysis, and bioreactance. These methods take advantage of measuring pulse pressure or stroke volume and their variation during the respiratory cycle, where increases and decreases in venous return produce subtle changes in cardiac output. While these methods of predicting fluid responsiveness have been shown to perform well, they require invasive blood pressure monitoring as well as proprietary devices (eg, PiCCO, FloTrac™, NICOM™) which are not readily available in most emergency departments.10
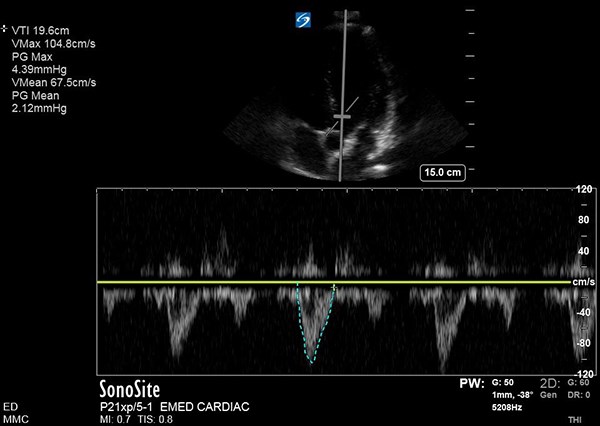
Echocardiography is a practical way for emergency physicians to determine if fluid therapy will increase cardiac output. Echo- cardiography can predict fluid responsiveness by measuring stroke distance, also known as the velocity time integral (VTI), before and after a passive leg raise (PLR). VTI is a measure of the distance blood travels during a cardiac cycle, and serves as a surrogate for stroke volume.11 VTI can be measured in patients who are mechanically ventilated, spontaneously breathing, and with dysrhythmia. Increases in VTI induced by a PLR indicate a patient is fluid responsive.
Emergency physicians can accurately measure VTI.12 Dr. Avila at 5 Minute Sono demonstrates how to perform this technique at the bedside.13 The technique and its limitations are also described by Marsia Vermeulen in the November 2017 edition of EM Resident.14
From the apical four chamber view, an apical five chamber view can be obtained by angling the probe anteriorly. The pulsed-wave doppler gate is then placed over the aortic outflow tract and a biphasic waveform is generated. On many ultrasound machines, the VTI is auto- calculated after the waveform is traced. The VTI is measured before and 1-2 minutes after PLR. Preload is augmented by PLR. If VTI increases after PLR, one can infer that the patient's stroke volume, and therefore cardiac output and MAP, will increase with a fluid bolus. If VTI does not increase, the patient may be better served with vasopressors or inotropes. One study demonstrated that an increase in VTI by 12.5% was 77% sensitive and 100% specific for response to a 500mL fluid bolus.15 Another study demonstrated that in increase in VTI of 10% after PLR was 97% sensitive and 94% specific for fluid responsiveness.16
Fluid administration is an integral part of resuscitation in the critically ill patient; however, only 50% of unstable patients will respond to a fluid bolus. Both under-resuscitation and hypervolemia are harmful to patients. VTI is the most accurate bedside tool to guide the resuscitation of your critically ill patients and predict if they will respond to a fluid bolus.
References
1. Bentzer P, Griesdale DE, Boyd J, Maclean K, Sirounis D, Ayas NT. Will This Hemodynamically Unstable Patient Respond to a Bolus of Intravenous Fluids? JAMA. 2016;316(12):1298-309.
2. Lehman LW, Saeed M, Talmor D, Mark R, Malhotra A. Methods of blood pressure measurement in the ICU. Crit Care Med. 2013;41(1):34-40.
3. Walsh M, Devereaux PJ, Garg AX, et al. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology. 2013;119(3):507-15.
4. Corl KA, George NR, Romanoff J, et al. Inferior vena cava collapsibility detects fluid responsiveness among spontaneously breathing critically-ill patients. J Crit Care. 2017;41:130-137.
5. Muller L, Bobbia X, Toumi M, et al. Respiratory variations of inferior vena cava diameter to predict fluid responsiveness in spontaneously breathing patients with acute circulatory failure: need for a cautious use. Crit Care. 2012;16(5):R188.
6. Lanspa MJ, Grissom CK, Hirshberg EL, Jones JP, Brown SM. Applying dynamic parameters to predict hemodynamic response to volume expansion in spontaneously breathing patients with septic shock. Shock. 2013;39(2):155-60.
7. Barbier C, Loubières Y, Schmit C, et al. Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med. 2004;30(9):1740-6.
8. Feissel M, Michard F, Faller JP, Teboul JL. The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med. 2004;30(9):1834-7.
9. Moretti R, Pizzi B. Inferior vena cava distensibility as a predictor of fluid responsiveness in patients with subarachnoid hemorrhage. Neurocrit Care. 2010;13(1):3-9.
10. Mackenzie DC, Noble VE. Assessing volume status and fluid responsiveness in the emergency department. Clin Exp Emerg Med. 2014;1(2):67-77.
11. Armstrong W, Ryan T. Hemodynamics. In: Armstrong W, Ryan T (eds). Feigenbaum’s Echocardiography. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:218–241.
12. Dinh VA, Ko HS, Rao R, et al. Measuring cardiac index with a focused cardiac ultrasound examination in the ED. Am J Emerg Med. 2012;30(9):1845-51.
13. Avila J. Volume Responsiveness - LVOT VTI. 5 Minute Sono, 26 June 2017, 5minsono.com/lvot_vti.
14. Vermeulen M, Levin J. Management of Shock: Bedside Assessment of Cardiac Output. EM Resident. 2017;44(6):14-16.
15. Lamia B, Ochagavia A, Monnet X, Chemla D, Richard C, Teboul JL. Echocardiographic prediction of volume responsiveness in critically ill patients with spontaneously breathing activity. Intensive Care Med. 2007;33(7):1125-1132.
16. Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, Teboul JL. Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med. 2006;34(5):1402-1407.