Emphysematous pyelonephritis is a rare diagnosis in the ED but can be life-threatening.
Typically an evolution from ascending E. coli cystitis,1 its hallmark and namesake is intraparenchymal gas produced by necrotizing infection. Patients at higher risk for developing this condition include female patients and persons with diabetes (70%-90%),2-4 frequently with preexisting microvascular complications, such as diabetic neuropathy and nephropathy.4
Patients are typically ill-appearing and often present with flank pain, dysuria, pyuria, acute kidney injury, bacteremia, and sepsis.5,6 However, many present with more ambiguous abdominal symptoms, and the cause is elucidated only on imaging.6,7 Imaging is critical to the diagnosis and expeditious treatment of emphysematous pyelonephritis, as patients may need aggressive source control via nephrostomy tube, stent, or less commonly nephrectomy.8 We present a patient with an atypical presentation of emphysematous pyelonephritis.
Case
A 62-year-old female patient presented to the ED with a 4-day history of diffuse, vague abdominal pain. She reported pain primarily over the left upper quadrant and bilateral flanks, along with subjective fever, nausea, and emesis. She denied dysuria and hematuria. Past medical history was significant for long-standing hepatitis C, cirrhosis, and a recent diagnosis of hepatocellular carcinoma. She also had a history of unspecified liver surgery after a high-speed motor vehicle crash in the remote past.
Vitals on arrival demonstrated elevated blood pressure, tachycardia to the 100s, and temperature of 100.1°F. Physical exam revealed an uncomfortable patient with diffuse abdominal and flank tenderness. Initial lab testing was significant for a leukocytosis to 21.6 x 103/µL. Urinalysis was negative for nitrates, leukocyte esterase and bacteria; positive for protein +1, ketones, and hemoglobin +1.
The patient was started on IV fluids and broad-spectrum IV antibiotics.
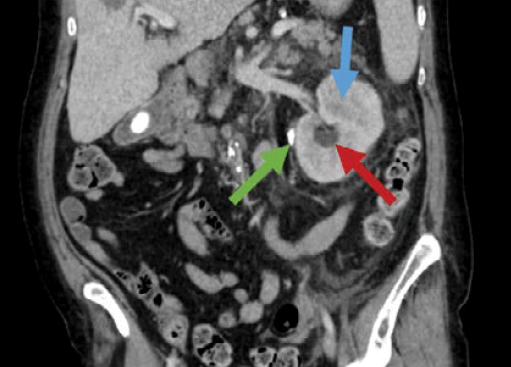
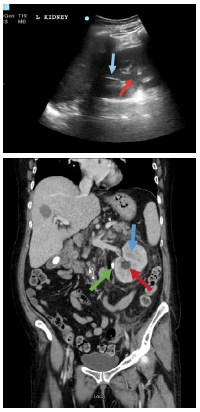
Abdominal point-of-care ultrasound demonstrated linear air with shadowing within the kidney parenchyma, concerning for emphysematous pyelonephritis.
When to Ultrasound?
Abdominal pain is a common presenting complaint in the emergency department.8 In the case of this patient with vague abdominal symptoms, without obvious urinary symptoms, and with a negative urinanalysis, suspicion for kidney stone or pyelonephritis was not particularly high, let alone the much rarer diagnosis of emphysematous pyelonephritis in a non-diabetic patient. POCUS is an excellent option that can be performed rapidly at the bedside, and for many cases of abdominal pathology including small bowel obstruction, cholecystitis, appendicitis, and obstructive renal processes may either inform the decision to proceed with CT or bypass it altogether.
When in doubt, pick up the ultrasound probe – a simple FAST exam along with survey of the kidneys and bowel can indicate some intraabdominal sources of sepsis along with free fluid, dilation of the bowel, and more.
Case Resolution
After diagnosis of emphysematous pyelonephritis was made, the patient was sent for nephrostomy tube placement with interventional radiology. Tube placement was uncomplicated and interval CT scan demonstrated decompression of the collecting system. Shortly after returning from the radiology suite, she decompensated precipitously, quickly becoming hypotensive despite fluid resuscitation and was started on vasopressors.
She was admitted to the ICU for ongoing management of sepsis secondary to emphysematous pyelonephritis, including IV antibiotics. Blood and urine cultures grew pan-sensitive E. coli, and IV antibiotics were deescalated to ceftriaxone. The patient improved significantly over the following 48 hours, transitioned to general care, and one week after admission the patient was discharged from the floor.
References
- Arsene C, Saste A, Arul S, Mestrovich J, Kammo R, Elbashir M, et al. A case series of emphysematous pyelonephritis. Case Rep Med. 2014;2014:587926.
- Smitherman KO, Peacock JE Jr. Infectious emergencies in patients with diabetes mellitus. Med Clin North Am. 1995 Jan;79(1):53-77. doi: 10.1016/s0025-7125(16)30084-0. PMID: 7808095.
- Schaeffer AJ. Infections of the urinary tract. In: Walsh PC, Retik AB, Vaughan ED, Wein AJ, Campbell M, editors. Campbell's Urology. 8th ed. Philadelphia, PA: Saunders; 2002. pp. 556–8.
- Lu YC, Chiang BJ, Pong YH, et al. Predictors of failure of conservative treatment among patients with emphysematous pyelonephritis. BMC Infect Dis. 2014;14:418. Published 2014 Jul 29. doi:10.1186/1471-2334-14-418
- Misgar RA, Mubarik I, Wani AI, Bashir MI, Ramzan M, Laway BA. Emphysematous pyelonephritis: A 10-year experience with 26 cases. Indian J Endocrinol Metab. 2016;20(4):475-480. doi:10.4103/2230-8210.183475
- Falagas ME, Alexiou VG, Giannopoulou KP, Siempos II. Risk factors for mortality in patients with emphysematous pyelonephritis: a meta-analysis. J Urol. 2007 Sep;178(3 Pt 1):880-5; quiz 1129. doi: 10.1016/j.juro.2007.05.017. Epub 2007 Jul 16. PMID: 17631348.
- Krishnamoorthy S, Zumla A, Sekar H, Muneer A, Thiruvengadam G, Kumaresan N. Prognostic scoring system and risk stratification in patients with emphysematous pyelonephritis: an 11-year prospective study at a tertiary referral centre. BJU Int. 2021 Apr;127(4):418-427. doi: 10.1111/bju.15225. Epub 2020 Oct 15. PMID: 32871043.
- Meltzer AC, Pines JM, Richards LM, Mullins P, Mazer-Amirshahi M. US emergency department visits for adults with abdominal and pelvic pain (2007-13): Trends in demographics, resource utilization and medication usage. Am J Emerg Med. 2017 Dec;35(12):1966-1969. doi: 10.1016/j.ajem.2017.06.019. Epub 2017 Jun 9. PMID: 28641981.