Electrical injuries range in severity from minor cutaneous burns to life-threatening internal organ damage and death. These injuries account for at least 30,000 non-fatal incidents and 1,000 fatalities in the U.S. every year.1
The mechanism of an electrical injury varies with age, with younger children accounting for household electrical injuries via cords and outlets, older children via high-voltage power lines, and adults via work-related accidents. Two-thirds of all electrical injuries occur in electrical and construction workers.2
CASE
A 20-year-old male was brought to the ED by EMS in cardiac arrest after an electrical injury while working as a residential construction worker. The patient was carrying an aluminum ladder that contacted overhead wires running to a house (240 volts). The homeowner had started CPR approximately 3 minutes after initial downtime. Upon EMS arrival, the patient was in ventricular fibrillation (VF). They delivered 4 rounds of defibrillation and 2 rounds of epinephrine en route to the ED, but attempts failed to achieve return of spontaneous circulation (ROSC). The estimated downtime prior to ED arrival was 25 minutes.
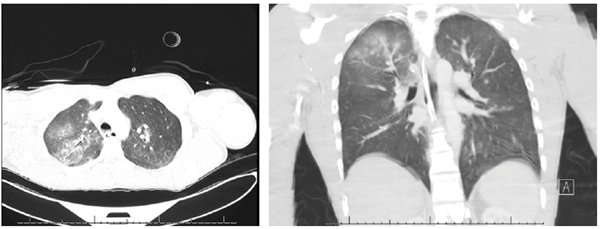
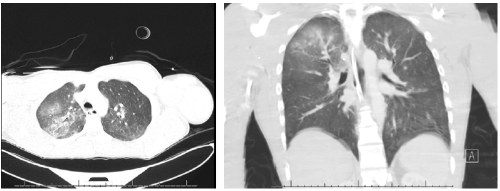
On arrival to the ED, the patient was in asystole with agonal respirations. He had a Glasgow Coma Scale of 3, no palpable pulses, cool extremities to touch, fixed and dilated pupils, and disconjugate gaze, with the right eye deviating laterally. Resuscitation was continued adhering to Advanced Cardiovascular Life Support guidelines. After the first round of CPR, VF was again detected, he was defibrillated, and ROSC was achieved with conversion to normal sinus rhythm. He was subsequently intubated. Vital signs were BP 164/80, HR 86, RR 16, T 35.6C (96.3°F), spO2 97%, on 35% FiO2. Secondary exam demonstrated erythema of the palmar aspect of the right hand, ecchymosis of the left popliteal fossa, and bilateral great toe linear "exit wound" burns with necrotic centers. His EKG showed wide QRS complexes with nonspecific ST-T changes. Chest x-ray and chest CT showed right upper and middle lobe pulmonary contusions.

Upon returning from imaging, he was noted to have equal and reactive pupils with aligned gaze. During the remainder of his ED stay, telemetry showed fluctuations from atrial fibrillation to sinus tachycardia, but no further chemical or electrical interventions were required.
DISCUSSION
There are 2 types of electrical current: direct current (DC) found in batteries and lightning, and alternating current (AC) used in electrical wires. AC and DC can be further categorized into low-voltage (<1,000 volts) or high-voltage (>1,000 volts). When traveling through the human body, the current follows the path of least resistance. This resistance is variable based on the type of organ or tissue it is going through with the highest to lowest resistance being bone, fat, tendon, skin, muscle, blood vessel, and nerve.3 The severity of the injury due to low-voltage AC can be increased by tetany causing prolonged contact, which is seen more in low voltages, as compared to higher voltage DC that may cause one large single muscle contraction. Many different organ systems are affected by an electrical injury, but we are going to limit the discussion to those injured in our patient.
CARDIOVASCULAR
The heart is the internal organ most commonly affected by electrical injury as it is located along many paths between entrance and exit of the electrical current.4 Cardiac injuries can occur due to direct damage from the electrical current to the myocardium, extensive catecholamine release, myocardial infarction, severe hypotension leading to hypoperfusion, and myocardial contusion due to prolonged CPR. EKG findings may demonstrate arrhythmias, myocardial damage, and conduction abnormalities. Typically, high-voltage DC causes ventricular asystole and AC causes death via VF. Delayed arrhythmias after an initial presentation of NSR have been seen up to 12 hours later.5
It is important to note that normal cardiac markers cannot rule out heart damage, as shown in our patient who had normal CK and troponin levels despite clear signs of myocardial injury. There should be high suspicion that the electrical pathway may have cardiac involvement in cases with loss of consciousness or entrance wounds on the hands. The most significant clinical predictor of cardiac injury is evidence of a vertical pathway of electricity, mapped by a line between the entrance and exit wounds.6 Our patient was found to have a vertical pathway between his right hand and feet.
NERVOUS
Neurological deficits can be present throughout the central (CNS) and peripheral (PNS) nervous systems, often due to cerebral hemorrhage and infarction. The etiologies of these injuries may include but are not limited to direct damage, thermal damage, tissue separation whether due to electrostatic measures or force, and ischemic changes.7 Acute-onset neurological deficits have a more favorable outcome than those which are delayed.8 Immediate injuries are typically seen in the CNS with loss of consciousness as well as respiratory and motor paralysis. Delayed injuries are more often documented in high-voltage injuries with spinal cord injuries taking as little as a few hours and up to a few years to present.9 Albeit rare, these long-term effects have included amyotrophic lateral sclerosis and other demyelinating disorders.7 Dysfunction of cranial nerves associated with the eye as seen in our patient can occur due to reversible autonomic deficits and should not be used as indication of poor prognosis.10
RESPIRATORY
Pulmonary injuries rarely present after a low or high voltage contact and are more often seen after a lightning strike. Our patient showed multiple pulmonary contusions on chest CT in his right upper and middle lobes. As he had no previous pulmonary disease, no signs of thoracic or abdominal wall trauma, or concern for respiratory infection, we suspect the pulmonary contusions were most likely caused by electrical injury, specifically the flow of electricity from his right hand to his lungs. In addition, prolonged tetany of the diaphragm and intercostal muscles may have contributed to his respiratory arrest. The pathology is consistent with two other cases describing low-voltage pulmonary contusions, making this the third case reported in English literature worldwide.11,12 These injuries can be a result of either non-thermal effects (electricity causing cellular changes) or due to thermal effects (electricity heating surrounding air causing a blast).
Other low-voltage pulmonary injuries have included cardiogenic and neurogenic induced pulmonary edema as well as ground-glass opacities with thickening of interlobular septa and bronchial walls. With high-voltage electrical injuries, pulmonary embolism and infiltrates have been described.12-16
INTEGUMENTARY
The severity of skin manifestations after an electrical injury can vary, but it is important to recognize that the level of cutaneous involvement is a poor predictor of the extent of internal injury. When present, burn marks are more commonly seen at the point of contact and where the electrical current exited the individual.1 Our patient was noted to have an entrance wound on his right palm and bilateral exit wounds on his big toes. Kissing burns may also be seen in individuals as a result of limb flexion and the electricity arcing from one surface to another.17 An electrical burn can be treated similarly to a thermal injury.
CASE RESOLUTION
After being stabilized in our community ED, the patient was transferred to a burn center. Prior to transfer, he began to have spontaneous movements requiring sedation. Upon arrival at the burn center, the patient was subsequently cooled secondary to VF arrest. By the end of hospital day one, he was more alert and was extubated without issue. His hospital course was complicated by elevated troponin levels, but he was ultimately cleared by cardiology and discharged from the hospital four days later with full neurologic recovery.
TAKE-HOME POINTS
- Limited external injuries should not limit a thorough evaluation for internal injuries.1
- Ocular dysfunction should not be used as an indicator of poor patient outcome.10
- Cardiac insults should be considered with low voltage electrical injuries.5
REFERENCES
- Zemaitis MR, Foris LA, Lopez RA, Huecker MR. Electrical Injuries. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448087/. Published January 2020.
- Pinto D, Clardy P. Environmental and Weapon Related Electrical Injuries. UpToDate. https://www.uptodate.com/contents/environmental-and-weapon-related-electrical-injuries. Published 2020.
- Miller BK, Goldstein MH, Monshizadeh R, Tabandeh H, Bhatti MT. Ocular Manifestations of Electrical Injury: A Case Report and Review of the Literature. CLAO Journal. 2002;28(4):224-227. doi: 10.1097/01.ICL.0000032345.79593.24
- Waldmann V, Narayanan K, Combes N, Marijon E. Electrical injury. BMJ. April 2017. doi:10.1136/bmj.j1418
- Waldmann V, Narayanan K, Combes N, Jost D, Jouven X, Marijon E. Electrical cardiac injuries: current concepts and management. European Heart Journal. 2017;39(16):1459-1465. doi:10.1093/eurheartj/ehx142
- Chandra NC, Siu CO, Munster AM. Clinical predictors of myocardial damage after high voltage electrical injury. Critical Care Medicine. 1990 Mar;18(3):293-7. doi: 10.1097/00003246-199003000-00010.
- Andrews C, Reisner A. Neurological and neuropsychological consequences of electrical and lightning shock: review and theories of causation. Neural Regeneration Research. 2017;12(5):677. doi:10.4103/1673-5374.206636
- Parvathy G, Shaji CV, Kabeer KA, Prasanth SR. High-voltage electrocution causing bulbar dysfunction. Journal of Neurosciences in Rural Practice. 2016;07(03):453-455. doi:10.4103/0976-3147.181479
- Koller J, Orságh J. Delayed neurological sequelae of high-tension electrical burns. Burns. 1989;15(3):175-178. doi: 10.1016/0305-4179(89)90175
- Hanson GC, Mcilwraith GR. Lightning Injury: Two Case Histories and a Review of Management. BMJ. 1973;4(5887):271-274. doi:10.1136/bmj.4.5887.271
- Karamanli H, Akgedik R. Lung damage due to low-voltage electrical injury. Acta Clinica Belgica. 2017 Oct;72(5):349-351. doi: 10.1080/17843286.2016.1252547
- Chen CW, Lin YK, Yeh YS, Chen CW, Lin TY, Chang SH. Low-Voltage Electricity-Associated Burn Damage of Lung Parenchyma: Case Report and Literature Review. Journal of Emergency Medicine. 2020 Oct 20:S0736-4679(20)30975-6. Doi: 10.1016/j.jemermed.2020.09.039.
- Schein RM, Kett DH, De Marchena EJ, Sprung CL. Pulmonary edema associated with electrical injury. Chest. 1990;97(5):1248-1250. doi: 10.1378/chest.97.5.1248
- Masanès MJ, Gourbière E, Prudent J, et al. A high voltage electrical burn of lung parenchyma. Burns. 2000;26(7):659-663. doi: 10.1016/S0305-4179(00)00035-8
- Schleich AR, Schweiger H, Becsey A, Cruse CW. Survival after severe intrathoracic electrical injury. Burns. 2010;36(5):e61-4. https://doi.org/10.1016/j.burns.2009.06.207
- Truong T, Le TV, Smith DL, Kantrow SP, Tran VN. Low-voltage electricity-induced lung injury. Respirology Case Reports. 2017;6(2). doi:10.1002/rcr2.292
- Krisna M. Electrical burn. Electrical burn | DermNet NZ. https://dermnetnz.org/topics/electrical-burn. Published September 2015. Accessed December 2, 2020.