Case
An 83-year-old male with a past medical history of hypertension, hyperlipidemia, and Parkinson's dementia presents to the emergency department for acute onset shortness of breath. Upon arrival, he was tachypneic with an oxygen saturation of 70% on room air. What is your interpretation of his ECG?
Answer
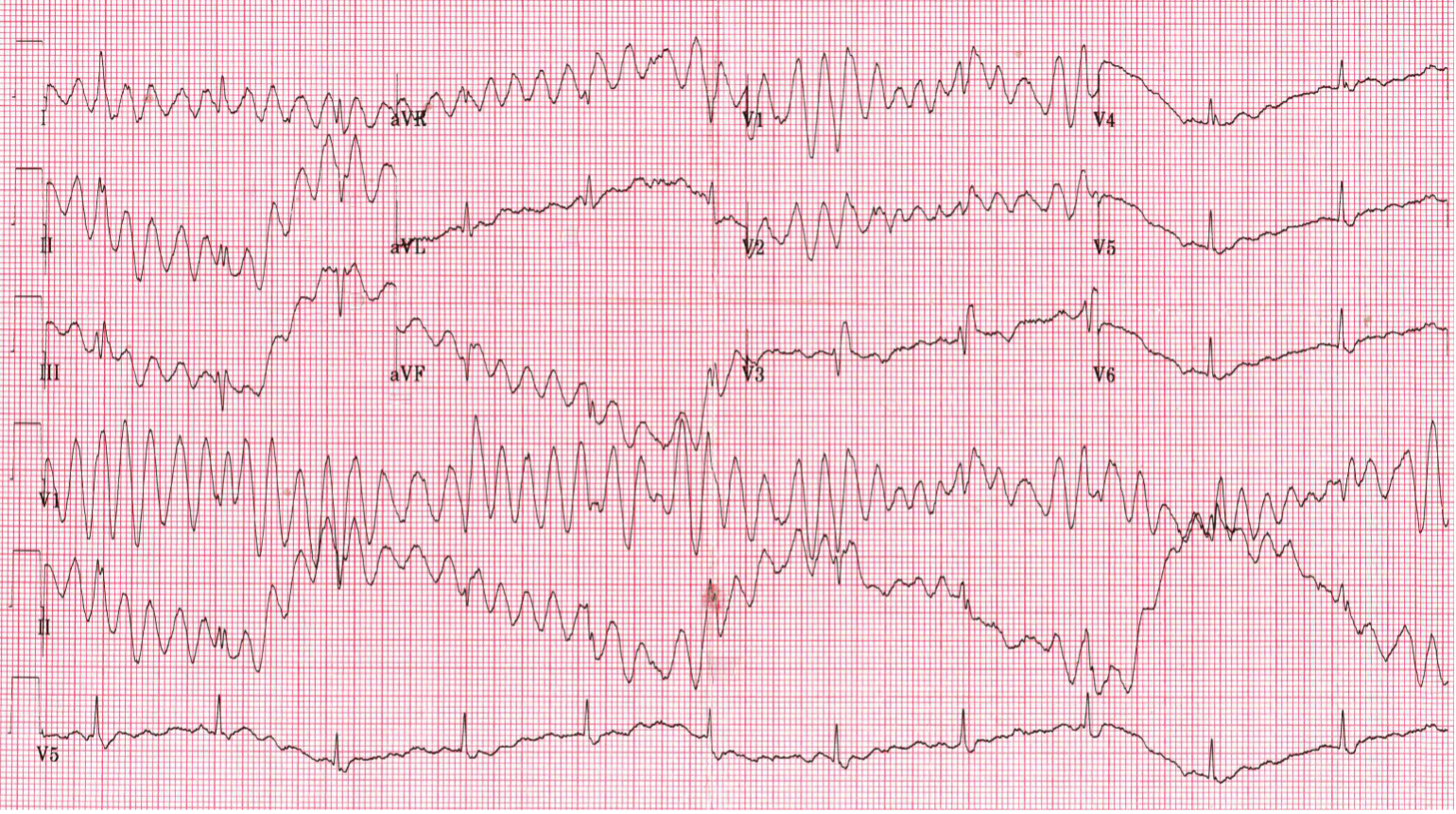
This ECG shows normal sinus rhythm at 65 bpm, best seen in leads aVL and V3-V6. There is also likely a right bundle-branch block, best seen in lead V3. The remaining limb leads and leads V1-V2 show an irregular wide complex tachycardia with an average ventricular rate of 320 bpm, no discernible P-waves, and phasic variation (ie, happens over a number of beats) of the QRS complex axis and amplitude. These findings are consistent with pseudo-ventricular tachycardia, which describes when artifact mimics polymorphic VT.
Discussion
Pseudo-ventricular tachycardia occurs when electrocardiographic artifact mimics polymorphic VT. In this case, the artifact is due to the patient’s Parkinsonian tremors. These are a common cause of ECG artifact and prone to misinterpretation and subsequent unnecessary interventions.1
ECG artifact can be broadly classified as pseudo-arrhythmic or non-arrhythmic. Pseudo-arrhythmic artifact can mimic a variety of dysrhythmias, including ventricular tachycardia, atrial fibrillation, and atrial flutter.2 Non-arrhythmic artifact can lead to misinterpretation of Q-waves, ST-segments, and T-waves. The most common causes of pseudo-arrhythmic artifact are body movement and poor skin-electrode contact.2 Misinterpretation of ECG artifact affects not only EM physicians, but also cardiologists and electrophysiologists.2 In one paper from the New England Journal of Medicine, 12 patients underwent unnecessary diagnostic testing, admission, or interventions based on misdiagnosis of ECG artifact.2,3
It is very important to differentiate pseudo-ventricular tachycardia from true pathologic dysrhythmias. When examining a single-lead telemetry strip or cardiac monitor, concern for significant dysrhythmia should prompt checking alternate leads or obtaining a 12-lead ECG.2,3 It also may be beneficial for the clinician to be at bedside to observe the patient’s movements while the ECG is being recorded.
There are 3 signs that can help identify pseudo-VT on an ECG:4
- The sinus sign: the presence of normal P-QRS-T complexes in either a limb or augmented lead that is due to one of the upper limb electrodes being free of movement artifact. This is best seen in lead V5 on the case ECG.
- The spike sign: the presence of regular or irregular spikes throughout the pseudo-VT that is due to the superimposition of the underlying normal sinus rhythm. This is best seen in lead I on the case ECG.
- The notch sign: the presence of a superimposed notch on the pseudo-VT that is due to the superimposition of the underlying normal sinus rhythm. This is best seen in lead II on the case ECG.
Case Conclusion
This patient was found to have pneumonia and was admitted to the internal medicine service for further treatment.
Pseudo-ventricular Tachycardia Learning Points
- Artifact is common, so all ECG leads should be analyzed in their entirety to rule out artifact-related abnormalities.
- A manually checked pulse should correlate with the rate on the ECG, rhythm strip, or cardiac monitor.
- Parkinsonian tremors disproportionately affect the limb leads more than the precordial leads.
- Misinterpretation of artifact can lead to unnecessary interventions.
- The sinus sign, spike sign, and notch sign can help identify artifact-related dysrhythmias.
References
- Hwang WJ, Chen JY, Sung PS, Lee JC. Parkinsonian tremor-induced electrocardiographic artifacts mimicking atrial flutter/fibrillation or ventricular tachycardia. Int J Cardiol. 2014;173(3):597-600.
- Knight BP, Pelosi F, Michaud GF, Strickberger SA, Morady F. Clinical Consequences of Electrocardiographic Artifact Mimicking Ventricular Tachycardia. N Engl J Med. 1999;341(17):1270-1274.
- Osman W, Hanson M, Baranchuk A. Pseudo–Ventricular Tachycardia, Pseudo–Atrial Fibrillation, and Pseudo–Atrial Flutter in a Patient With Parkinson Disease: Two’s Company, Three’s a Crowd. JAMA Int Med. 2019;179(6):824-826.
- Huang CY, Shan DE, Lai CH, et al. An accurate electrocardiographic algorithm for differentiation of tremor-induced pseudo-ventricular tachycardia and true ventricular tachycardia. Int J Cardiol. 2006;111:163-165.



