A 22-year-old female with no significant past medical history presents to the emergency department with wheezing after a recent upper respiratory infection. The patient is treated with a continuous 15 mg albuterol nebulizer, after which an ECG is obtained. The patient’s respiratory status has significantly improved, and she has no new symptoms. What is your interpretation of her ECG?
Answer
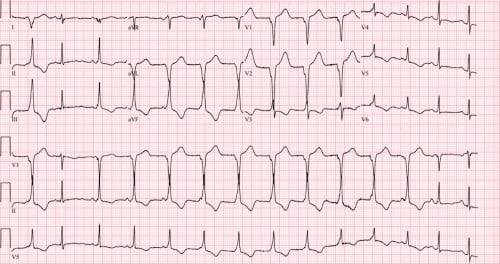
This ECG shows normal sinus rhythm at ~75 bpm followed by a regular wide complex rhythm at ~83 bpm before resuming normal sinus rhythm.
The regular wide complex rhythm starting with the 7th QRS complex is consistent with an accelerated idioventricular rhythm (AIVR), which occurs due to increased automaticity or triggered activity of a ventricular pacemaker. AIVR is commonly seen after successful reperfusion, partial or complete, of an occluded coronary vessel. The reperfusion can be spontaneous or due to an intervention such as PCI or fibrinolysis.
Other causes of AIVR include beta-sympathomimetics (as in this case), digoxin toxicity, cocaine, electrolyte abnormalities, cardiomyopathy, myocarditis, or an athletic heart with increased vagal tone.1,2 In the past, AIVR has been referred to as non-paroxysmal ventricular tachycardia, isorhythmic slow ventricular tachycardia, and our favorite, “the curious benevolent tachycardia.”
The classic teaching is that AIVR has rates between 40 and 110 bpm and VT has rates between 140 and 200 bpm, but these numbers are not strict limits. AIVR can be seen with rates as high as 130 bpm and VT can be seen with rates as slow as 120 bpm (and even slower in patients on chronic oral antidysrhythmic medications or those with severe cardiomyopathies). Although the ventricular rate in this ECG is consistent with AIVR, it's important not to anchor on the ventricular rate as the sole factor to differentiate AIVR from VT.
Another key finding in this ECG is the presence of AV dissociation in the absence of a 3rd degree, or complete, AV block. It is important to differentiate a 3rd degree AV block from AV dissociation. A 3rd degree AV block describes the absence of conduction from the atria to the ventricles via the AV node. AV dissociation describes when the atria and ventricles operate independently of each other. A 3rd degree AV block will always have AV dissociation, but there can be AV dissociation without a 3rd degree AV block (e.g., ventricular tachycardia, decreased SA node automaticity such that a junctional or ventricular site takes over pacing, or if, like this case shows, there is increased automaticity in a junctional or ventricular site that is faster than the SA node). In these cases, the AV node functions normally, but the impulses from the SA node are blocked by the retrograde conduction from the faster junctional or ventricular pacing.
Associated ECG findings seen with AV dissociation include capture and fusion beats. A capture beat is a sinus P-QRS-T complex formed by transient normal conduction amid AV dissociation. A fusion beat is caused by the simultaneous depolarization of the ventricle from both a normal supraventricular focus (e.g., a sinus beat from the SA node) and a ventricular focus. The 3rd QRS complex in this ECG, best seen in the lead II rhythm strip, is an example of a fusion beat.
AIVR is typically transient, often lasting only minutes, and unlikely to cause hemodynamic instability. In most circumstances, there is no treatment required except for observation. Patients with decreased cardiac output may benefit from a trial of atropine to increase the SA node rate in order to restore AV synchrony and the atrial kick.4 Special consideration should be taken in the patient with apparent AIVR who presents with syncope as this could be a sign of a more malignant underlying cardiac issue.
Case Conclusion
This patient was discharged after successful treatment of her respiratory symptoms.
Accelerated Idioventricular Rhythm Learning Points
- Ectopic focus from Purkinje network or ventricular myocardium
- Also called ventricular escape rhythm
- ECG shows ≥ 3 consecutive, regular, wide complex beats with no P-waves or AV dissociation if P-waves are present
- Rates between 40-110 bpm, but can sometimes be as high as 120-130 bpm
- Mimics include hyperkalemia, sodium channel blocker toxicity, and VT in patients on antidysrhythmic medications (e.g., amiodarone, flecainide, sotalol) or with severe cardiomyopathies
- Suggests partial or complete reperfusion of an occluded coronary vessel
- Classically seen in the reperfusion phase of an MI following fibrinolysis or PCI, but can also be spontaneous
- Can also be seen with digoxin toxicity, cardiac ischemia, or electrolyte abnormalities
- Usually well-tolerated, benign, and self-limiting
- Treating as VT with antidysrhythmic medications can precipitate asystole
References
- Gildea TH, Levis JT. ECG Diagnosis: Accelerated Idioventricular Rhythm. Perm J. 2018;22:17-173.
- Rothfeld EL, Zucker IR, Parsonnet V, Alinsonorin CA. Idioventricular rhythm in acute myocardial infarction. Circulation. 1968;37(2):203–209.
- Riera AR, Barros RB, de Sousa FD, Baranchuk A. Accelerated idioventricular rhythm: history and chronology of the main discoveries. Indian Pacing Electrophysiol J. 2010;10(1):40-48.
- Scheinman MM, Thorburn D, Abbott JA. Use of atropine in patients with acute myocardial infarction and sinus bradycardia. Circulation. 1975;52(4):627–633.



