CASE
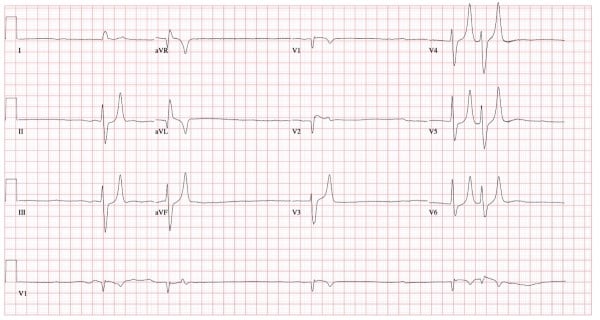
A 74-year-old male with a PMH of HTN, CKD, and HFpEF presents with exertional weakness and near-syncope for the past 2 days. What is your interpretation of his ECG?
ANSWER
This ECG shows and irregularly irregular bradycardia with a ventricular rate of 30 bpm, near-absent P-waves, left axis deviation, prolonged QRS complex duration, STE in leads in V1-V2, and peaked T-waves in leads II, III, aVF, and V3-V6.
Possible etiologies of an irregular bradycardia include atrial fibrillation with slow ventricular response, atrial flutter/tachycardia with slow ventricular response, wandering atrial pacemaker, 2nd degree AV block Mobitz types I and II, variable high-grade AV block, and sinus bradycardia or junctional rhythm/bradycardia with regular/irregular pattern of PAC, PJC, and/or PVC. The rhythm in this ECG does not meet the criteria for any of these rhythms, and the findings of severe bradycardia, bizarre rhythm, peaked T-waves, and prolonged QRS complex duration are concerning for hyperkalemia.
Hyperkalemia typically causes ECG changes when the serum potassium level reaches approximately 6 mEq/L, however there is poor correlation between ECG features and the degree of hyperkalemia.1 Although the most severe cardiac manifestations of hyperkalemia have been shown to regularly occur with potassium concentrations greater than 9 mEq/L, ECG abnormalities do not always correlate reliably with serum potassium levels and clinical decompensation can occur without profound changes in potassium concentration. In other words, the ECG has poor sensitivity and specificity for hyperkalemia and cardiac death due to hyperkalemia. Hyperkalemia can also mimic STEMI (typically anterior), Brugada syndrome, and DeWinter’s T-waves.1,4,5
The pathophysiology behind the ECG changes seen with hyperkalemia relates to the importance of extracellular potassium in regulating the cardiac membrane potential. Initially, the increased extracellular potassium leads to increases in myocardial excitability and conduction velocity, resulting in peaked T-waves and increased risk of tachydysrhythmias.1,2,5 As potassium levels rise further, the opposite happens- the conduction velocity decreases and the refractory period increases. The decreasing conduction velocity manifests on a 12-lead ECG as if the entire P-QRS-T complex were being pulled at both ends like a string, eventually leading to the classic sine wave pattern. The increase in refractory period can precipitate development of bradydysrhythmias such as sinus bradycardia, high grade AV blocks, and atrial fibrillation with slow ventricular response. These pro-arrhythmogenic effects can lead toventricular tachycardia/fibrillation, PEA, or asystole.2,3,4,5
The initial treatment for hyperkalemia includes calcium gluconate or calcium chloride. It is important to understand how calcium stabilizes the membrane in order to monitor its effect on the EKG to guide treatment. Calcium hyperpolarizes the cardiac membrane which is why hypercalcemia can lead to a short QT interval with STE that mimics an AMI. When hyperkalemia is severe enough to hypopolarize the cardiac membrane (ie, everything on the ECG is prolonged), calcium counteracts this affect and brings the resting membrane potential back to normal, thus mitigating the risk of bradydysrhythmias and subsequent decompensation. The effect of calcium should be evident on the ECG if appropriately dosed. It’s important to note that this may not be the case if the ECG only shows peaked T-waves since this is a hyperpolarized state. That said, it is still reasonable to give calcium if there are only peaked T-waves in anticipation of worsening hyperkalemia and the associated hypopolarized state.
CASE CONCLUSION
The patient’s initial labs were notable for a potassium of 8.4 mEq/L thought to be secondary to acute kidney injury in the setting of recement initiation of ACE-I therapy. He was taken for emergent dialysis for definitive treatment.
Hyperkalemia Learning Points
- ECG is specific but not sensitive for hyperkalemia
- ECG changes are not always sequential/progressive and include:
- Tall, narrow, peaked T-waves (best seen in precordial leads)
- P-wave flattening and PR interval prolongation
- Prolonged QRS complex duration, ranging from minimal to maximal
- Conduction abnormalities (AV blocks, fascicular and bundle branch blocks)
- Bradycardia
- Sino-ventricular rhythm (loss of P-waves, extremely widened QRS) with normal or slow rate
- Ventricular dysrhythmias
- Can cause STE (common in leads V1-V2 and aVR) that mimics STEMI or Brugada pattern
- Can occur simultaneously with hyperacute T-waves and obscure early changes seen in an anterior or anteroseptal AMI
- The “syphilis of ECG abnormalities,” meaning that a broad range of abnormalities can be encountered with hyperkalemia6
REFERENCES
- Hunter RW, Bailey MA. Hyperkalemia: pathophysiology, risk factors and consequences. Nephrol Dial Transplant. 2019;34(Suppl 3):iii2-iii11.
- Hanumanthu BKJ, Chugh Y, Grushko M, Faillace RT. Hyperkalemia Presenting as Sinus Bradycardia, Junctional Rhythm and Atrial Bigeminy. Cureus. Published online December 21, 2019.
- Buttner R, Burns E. Hyperkalaemia. Life in the Fast Lane • LITFL. Published August 1, 2018. Accessed September 15, 2023. Available at https://litfl.com/hyperkalaemia-ecg-library/.
- McLaren J. EM Cases | ECG Cases 10: hyperkalemia. Emergency Medicine Cases. Published June 16, 2020. Accessed September 15, 2023. Available at https://emergencymedicinecases.com/ecg-cases-10-hyperkalemia-the-great-imitator/.
- Littmann L, Gibbs MA. Electrocardiographic manifestations of severe hyperkalemia. J Electrocardiol. 2018;51(5):814-817.
- Mattu A. ECG Weekly. Available at www.ecgweekly.com.



