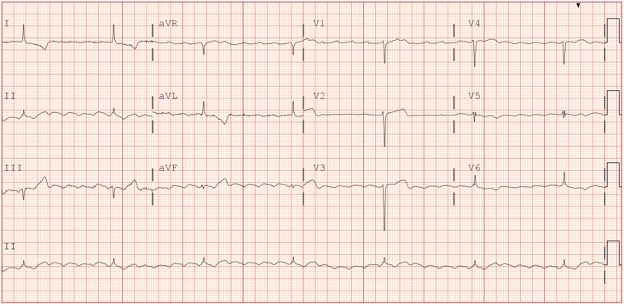
A 70-year-old male presents to the emergency department with syncope and lightheadedness. His past medical history is significant for heart failure with reduced ejection fraction, CAD status post percutaneous coronary intervention, hypertension, and paroxysmal atrial fibrillation on apixaban. What is your interpretation of his ECG?
Answer
This ECG shows atrial flutter with 6:1 conduction and a ventricular rate of ~42 bpm, normal axis, normal QTc interval, poor R-wave progression, and ST-segment and T-wave abnormalities in leads I, aVL, and V1-V3 suggestive of LVH with strain pattern.
This ECG shows flutter waves, also called F-waves, best seen in the inferior leads, that are diagnostic of atrial flutter. Atrial flutter is typically due to a re-entry circuit around the tricuspid ring in the right atria. It is classified as a macro-reentry tachycardia because it revolves around a large obstacle, the right atrium, as opposed to a small obstacle like the AV node. The concerning finding in this ECG is the bradycardic ventricular rate, which is likely the cause of the patient’s symptoms. Important intrinsic causes to consider include fibrosis/sclerosis of the conduction system, MI, ischemic heart disease, and infiltrative/inflammatory disorders (eg, cardiac amyloidosis, myocarditis). Important extrinsic etiologies to consider include antidysrhythmic medication toxicity (eg, digoxin, beta-blockers, CCB, etc.) and electrolyte abnormalities (eg, hyperkalemia).
Regarding the findings suggestive of LVH, it is important to note that none of the many diagnostic ECG criteria for LVH have great sensitivity, so while anatomic LVH can lead to characteristic changes seen on ECG, it is ultimately an echocardiographic diagnosis. ECG findings that are characteristic of the LVH strain pattern include a large S-wave with STE and a concave upward ST-segment in leads V1-V3, and a large R-wave with STD, TWI, and a concave downward ST-segment in leads I, aVL, and V4-V6.
Conclusion
The patient was successfully cardioverted to normal sinus rhythm then admitted to the cardiology service for placement of a permanent pacemaker. The patient’s slow ventricular response was suspected to be caused by atrioventricular node dysfunction secondary to age-related fibrosis of the conduction system.
Atrial Flutter Learning Points
- Due to a re-entrant circuit in the right atrium
- Stereotypical “sawtooth pattern” of P-waves seen best in the inferior leads
- Atrial rate is 250-350 bpm and typically fixed over time
- Ventricular rate is a fraction of atrial rate (i.e., for an atrial rate of 300 bpm, 2:1 conduction produces a ventricular rate of 150 bpm, 3:1 conduction produces a ventricular rate of 100 bmp, 4:1 conduction produces a ventricular rate of 75 bpm, etc.)
- Consider atrial flutter when ventricular rate is consistently around 150 bpm
- Vagal maneuvers or adenosine will affect the ventricular rate but not the flutter waves
- The risks of thromboembolism and recommendations for anticoagulation are the same for atrial flutter and atrial fibrillation1
- The American College of Cardiology (ACC) provides a Class I recommendation for elective synchronized cardioversion in stable patients pursuing a rhythm control strategy2
LVH Learning Points
- ECG is only suggestive of anatomic LVH, and echocardiography is the superior diagnostic modality
- ECG findings in LVH are manifested primarily by the increased voltage of the QRS complexes, hence the term “LVH by voltage criteria”
- No criteria are recommended for use exclusive of other validated criteria
- Diagnosis of LVH in the presence of intraventricular conduction abnormalities (eg, fascicular blocks, bundle branch blocks) should be made with caution as they may impact the accuracy of the ECG criteria for LVH
- LVH with strain pattern can confound the ECG’s ability to detect ACS, particularly anteroseptal MI, and mimics ACS findings
References
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society [published correction appears in J Am Coll Cardiol. 2019 Aug 20;74(7):1016-1018]. J Am Coll Cardiol. 2019;74(7):e51-e156. doi:10.1016/j.jacc.2018.10.044
- Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society [published correction appears in Circulation. 2016 Sep 13;134(11):e234-5]. Circulation. 2016;133(14):e506-e574. doi:10.1161/CIR.0000000000000311



