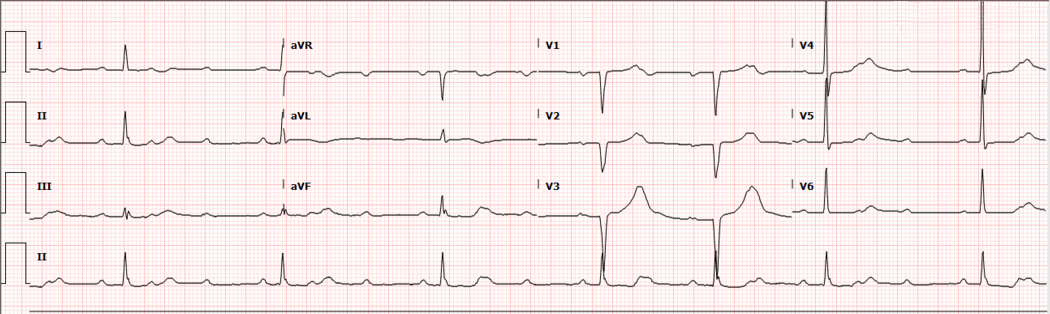
A 72-year-old female presents with exertional syncope for the past several days. What is your interpretation of her EKG?
High Degree AV Blocks
This ECG shows an irregular narrow complex bradycardia with a ventricular rate of ~40 bpm and a PR interval for the conducted P-waves is ~200 ms. The pattern of P waves and QRS complexes demonstrates a 3:1 AV block (QRS complexes 1, 2, 3, and 5) and a 2:1 AV block (QRS complexes 4 and 5). When interpreting an ECG with a 2:1 AV block, the absence of 2 consecutive conducted P waves makes it impossible to determine if the PR interval is lengthening or not. Since there is not enough information to determine if the underlying rhythm is a Mobitz I or Mobitz II, it is best to assume the higher risk Type II pathology. Note that while a wide QRS suggests a Mobitz Type II, a narrow QRS can be seen with both Type I and Type II. This ECG also shows a 3:1 AV block, which similarly to the 2:1 AV block, lacks 2 consecutive conducted P waves. 2nd degree AV blocks with ≥ 2 consecutive nonconducted P waves are called "high-grade" or "advanced" and are considered a variant of Mobitz Type II.
Image 2 shows a 4:1 AV block (there is a P wave buried in the T wave) with a ventricular rate of ~30 bpm and a RBBB with repolarization abnormalities in the right precordial leads. There are also STD in the inferior and lateral precordial leads of unclear etiology. Note that a RBBB will usually have STD and TWI in the right precordial leads, but only in leads that have a R'-wave. And unlike with a LBBB, the repolarization abnormalities associated with RBBBs do not include STE.
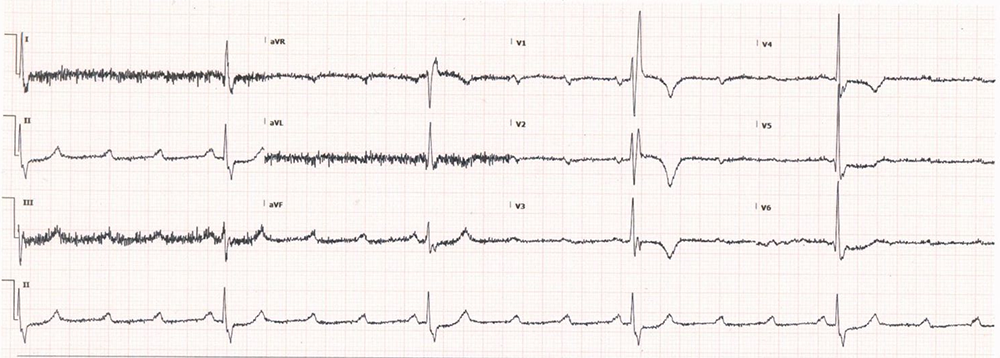
Although the changes seen in this ECG were not due to ischemia, it important to recognize that high-grade blocks, especially when there is a concurrent RBBB, are at high risk for decompensating into 3rd degree AV blocks and generally portend a poor prognosis when associated with anterior or anteroseptal MIs.
Learning Points
High-grade or Advanced 2nd Degree AV Block
GENERAL FEATURES
- Variant of Mobitz Type II where ≥ 2 sequential P waves are not conducted
EKG FEATURES
- ≥ 2 sequential P waves are not conducted
- Relatively constant PP interval
- Constant PR interval in conducted beats
- Described as ratio of P waves to QRS complexes
- QRS can be wide or narrow
CLINICAL SIGNIFICANCE
- Atropine is unlikely to lead to clinical improvement
- High risk of progression to 3rd degree AV block when associated with anterior or anteroseptal AMI
Right Bundle Branch Block (RBBB)
GENERAL FEATURES
- Delayed conduction through right ventricle with normal left ventricular conduction
EKG FEATURES
- QRS ≥ 120 ms
- Rsr’, rsR’, or rSR’ in V1 or V2
- S-wave duration > R-wave or > 40 ms in I and V6
- Normal R-wave peak time in V5 and V6 but > 50 ms in V1 (only required if a pure dominant R-wave +/- notch is present in V1)
CLINICAL SIGNIFICANCE
- Does not confound EKG evaluation of ACS (unlike LBBB)
- Repolarization abnormalities include ST depressions and T-wave inversions in V1-V3 ⇒ ischemia not easily determined in these leads
- The presence of axis deviation ⇒ evaluate for concurrent LAFB or LPFB
Case Conclusion
The patient’s workup in the ED, which included labs, troponins, and POCUS echocardiogram, was unremarkable. The patient was admitted to the Cardiology service for pacemaker placement and discharged after an uneventful hospital course.



