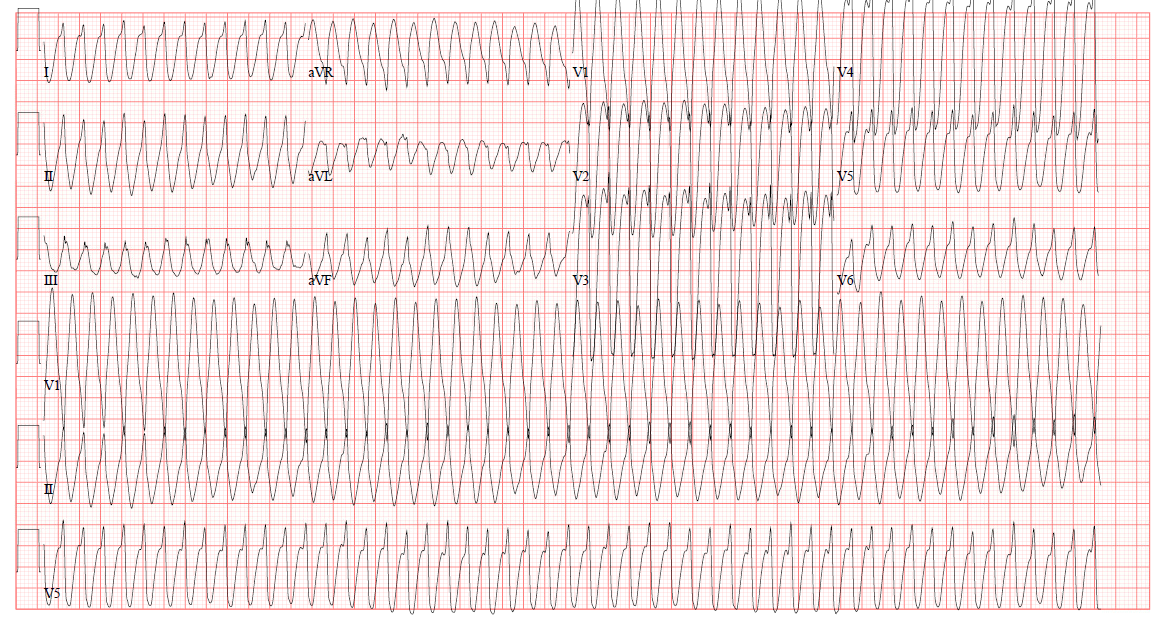
A 27-year-old male with a PMH of seizure disorder and developmental delay presents via EMS after a witnessed seizure. The patient was able to intermittently go into sinus rhythm with vagal maneuvers. What is your interpretation of his ECG?
Answer
This ECG shows a regular wide complex tachycardia with a ventricular rate of 315 bpm, no discernable P-waves, northwest/extreme axis deviation, and a prolonged QRS complex duration with an intraventricular conduction delay.
The differential diagnosis for a regular wide complex tachycardia includes:
- Monomorphic ventricular tachycardia
- Antidromic AVRT
- Any regular SVT (eg, sinus tach, AVNRT, atrial flutter, etc.) with aberrant conduction (eg, fixed or rate-related BBB, metabolic abnormalities, sodium channel blocker toxicity, etc.)
The patient's lack of risk factors (ie, young age, no cardiac history) and ability to break the rhythm with vagal maneuvers suggest a non-VT diagnosis (eg, AVNRT with aberrant conduction), but notable ECG findings that suggest VT include negative QRS concordance in leads V1-V6 (ie, all of the QRS complexes point down) and Brugada’s sign (ie, time from the onset of the QRS complex to the nadir of the S-wave is > 100 msec) best seen in leads V5-V6. These seemingly contradictory findings are often seen with idiopathic ventricular tachycardias.
Idiopathic ventricular tachycardias represent ~10% of all VTs and are generally seen in young, healthy patients in the absence of structural heart disease. Episodes of VT typically occur spontaneously but can be precipitated by infection, physical activity, or adrenergic stimulation. The majority of idiopathic VTs originate in the right ventricle, but 10-15% originate in the left ventricle.
Idiopathic fascicular ventricular tachycardia (IFVT), also known as verapamil-sensitive VT or Belhassen VT, is a re-entry tachycardia from an ectopic focus in the left ventricle. The ECG will show a RBBB-like pattern with a relatively mild prolongation of the QRS complex duration (120-140 msec). IFVT can easily be confused with SVTs with aberrant conduction. ECG findings that can help distinguish IFVT from SVT include capture beats, fusion beats, or AV dissociation. As the name verapamil-sensitive VT suggests, this rhythm is very responsive to verapamil, typically dosed 2.5-5 mg IV every 15-30 minutes. Common treatments for SVT (eg, adenosine and vagal maneuvers) are sometimes effective, which can lead to anchoring on a diagnosis of SVT.
The key learning point in this case is that responsiveness of a WCT to vagal maneuvers or nodal blocking medications is not diagnostic of SVT. From a therapeutic perspective, treating a WCT with adenosine is unlikely to cause the patient serious harm even if the underlying rhythm is VT. From a diagnostic perspective, it would be harmful to incorrectly diagnose the patient with SVT based on the response to adenosine when it was really VT.
Case Conclusion
This patient was effectively treated with IV procainamide and admitted to the cardiology service. His inpatient workup was notable for positive Lyme titers. He was treated for suspected Lyme carditis and discharged home on sotalol.
Monomorphic VT Learning Points
- ≥ 3 consecutive, regular, wide complex beats with rate > 120-130 bpm
- Non-sustained: < 30 sec duration with no hemodynamic instability
- Sustained: ≥ 30 sec duration OR causes hemodynamic instability
- Rates < 120-130 bpm can be seen in patients on chronic antidysrhythmic medications (eg, amiodarone, flecainide, sotalol) or with severe cardiomyopathies
- If rate < 120 bpm, consider mimics:
- Hyperkalemia
- Sodium channel blocker toxicity
- Accelerated idioventricular rhythm (AIVR)
ECG Features in a Regular WCT that Suggest VT
- QRS complex duration > 200 msec is almost always VT, hyperkalemia, or sodium channel blocker toxicity
- AV dissociation (ventricular rate > atrial rate)
- Positive or negative QRS complex concordance in leads V1-V6
- Extreme axis deviation (“northwest axis”)
- The absence of typical RBBB or LBBB pattern (ie, normal RBBB or LBBB pattern makes SVT with aberrant conduction more likely)
- Fusion beat: hybrid QRS complex formed by both supraventricular and ventricular focus
- Capture beat: sinus QRS complex formed by transient normal conduction amid AV dissociation
- Brugada’s sign: time from the onset of the QRS complex to the nadir of the S-wave is > 100 msec
- Josephson’s sign: notching on the downslope of the S-wave near its nadir



