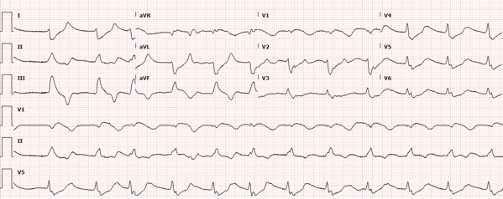
A 57-year-old male presents with AMS. He is minimally responsive and there is no additional history available. His initial heart rate was 25 with a blood pressure of 80/30. What is your interpretation of his ECG?
Answer
This ECG shows an irregular wide complex rhythm with an average ventricular rate of 72 bpm, right axis deviation, no discernable P-waves, and a prolonged QRS duration at 200 ms with an intraventricular conduction delay. These findings, in particular the very wide QRS complexes with bizarre morphologies, are consistent with hyperkalemia.
Hyperkalemia Presentation and Etiologies
Hyperkalemia is a common and a potentially life-threatening electrolyte disorder in patients presenting to the Emergency Department. Although severe cases may be associated with paralysis and cardiac arrest, symptoms in the majority of cases are nonspecific, including muscle pain/weakness, nausea, vomiting, and abdominal pain.1
The major causes of hyperkalemia can be categorized into two groups: conditions which impair the elimination of potassium, such as renal insufficiency or medications interfering with urinary excretion (spironolactone, NSAIDs, ACEI) and those conditions that cause the extracellular shift of potassium, such as digoxin or beta-blockers, acidosis, diabetes induced insulin decrease, and the tissue breakdown seen in rhabdomyolysis.
Hyperkalemia ECG Findings
The earliest electrocardiographic finding in hyperkalemia is typically peaked T waves. As serum potassium levels rise, the PR interval lengthens, P waves flatten and can eventually disappear entirely, and the QRS widens with the development of bizarre QRS morphologies. Severe hyperkalemia can lead to bradycardia, loss of SA nodal conduction, the development of the classic “sine wave” morphology, and, ultimately, asystole. In short, the ECG changes seen with hyperkalemia progress as if the entire P-QRS-T complex were being pulled at both ends like a string.
It is important to note that although the most severe cardiac manifestations of hyperkalemia have been shown to regularly occur at serum potassium concentrations greater than 9 mEq/L, ECG abnormalities do not always correlate reliably with serum levels and clinical decompensation can occur without profound changes in potassium concentration.2
Hyperkalemia Treatment
The initial goals in the treatment of hyperkalemia are stabilizing the cardiac membrane, promoting potassium influx into cells, and enhancing potassium excretion.
Calcium
- Temporarily stabilizes the cardiac membrane by counteracting potassium’s depolarizing effects
- Calcium gluconate via peripheral IV or calcium chloride if central venous access is obtained
- Dose: 1 amp of calcium gluconate (10 mL of 10% solution) every 3-5 min until ECG normalizes
- Onset of action: < 3 min
- Duration: ~20-50 min
Insulin and Dextrose
- Shifts potassium from serum into cells
- Effect is dose-dependent, and the dosage of dextrose should be adjusted per the patient’s serum glucose level and risk factors for hypoglycemia (renal insufficiency, use of medications for diabetes, etc.)
- Dose: 10 units regular insulin IV with 25-50 g (1-2 amps) 50% dextrose solution
- Onset of action: 10-30 min
- Duration: 2-6 hours
Albuterol
- Shifts potassium from serum into cells
- Usually given via a nebulizer and can be administered prior to obtaining IV access
- Dose: 10-20 mg nebulized over 10-30 min
- Onset of action: 15-30 min
- Duration: 2-4 hours
Diuretics and Dialysis
- Both eliminate potassium from the body
- Dialysis is the most effective and reliable method for the definitive treatment of hyperkalemia, especially for patients on dialysis
- Loop diuretics, such as furosemide, promote potassium excretion via the kidneys and can be considered in the appropriate clinical scenario
Cation Exchange Resins
- Includes sodium polystyrene sulfonate and patiromer
- Bind potassium in the GI tract to prevent absorption
- Onset of action is hours to days, so not indicated for acute hyperkalemia treatment
Of note, though bicarbonate was traditionally considered an element of the hyperkalemia treatment regimen, there is no literature to suggest a benefit when used in patients with hyperkalemia with normal pH. Bicarbonate infusions may have a role in the treatment of academia in patients who are concurrently hyperkalemic.
Case Conclusion
The patient’s initial labs were notable for a potassium of 7.9 mEq/L. This was treated with 3 g of calcium gluconate, 10 units of insulin, 1 amp of dextrose, and a 15 mg albuterol neb, after which his mental status and vital signs improved. A repeat ECG was obtained (see image) and showed resolution of the multiple abnormalities seen on his initial ECG. The patient was admitted to the hospital for further treatment of his hyperkalemia.
Repeat ECG after treatment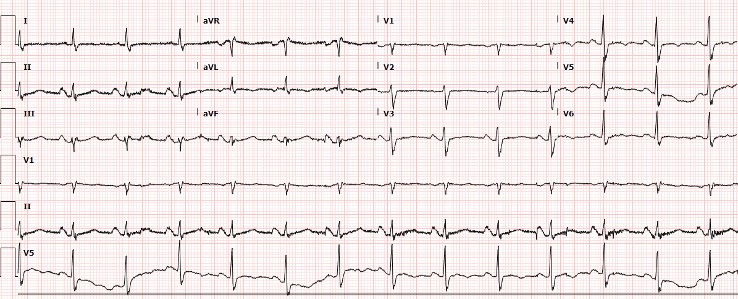
Hyperkalemia Learning Points
- EKG is specific but not sensitive for hyperkalemia
- EKG changes are not always sequential/progressive and include:
- Tall, narrow, peaked T-waves (best seen in precordial leads)
- P-wave flattening and PR interval prolongation
- Widened QRS with bizarre morphology
- Conduction abnormalities (AV blocks, fascicular and bundle branch blocks)
- Sinoventricular rhythm (loss of P-waves, extremely widened QRS) with normal or slow rate
- Ventricular dysrhythmias
- Treatment goals include:
- Stabilization of the cardiac membrane
- Promote potassium influx into cells
- Enhance potassium excretion
References
- Montague BT, Ouellette JR, Buller GK. Retrospective review of the frequency of ECG changes in hyperkalemia. Clin J Am Soc Nephrol. 2008;3(2):324-330.
- Parham WA, Mehdirad AA, Biermann KM, Fredman CS. Hyperkalemia revisited.Tex Heart Inst J. 2006;33(1):40-47.



