An 87-year-old female presents with generalized weakness for the past several days after a recent increase in her diuretic medication by her cardiologist.
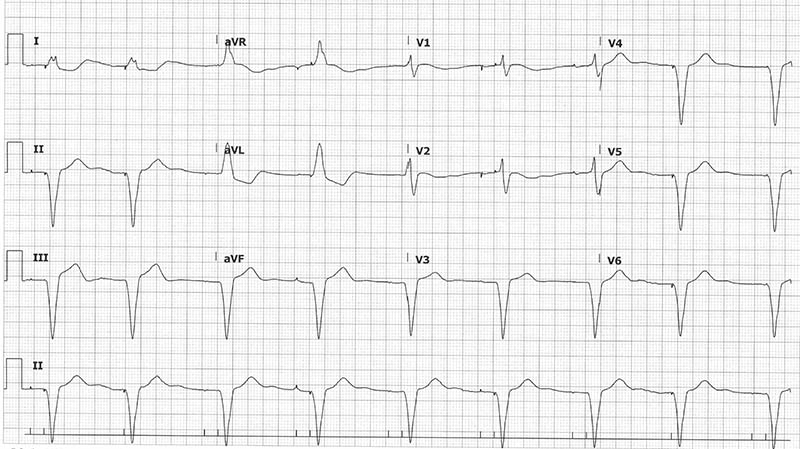
What is your interpretation of the following ECG? (Hint: there are 3 significant abnormalities.)
Pacemaker Malfunctions
This EKG shows an atrioventricular paced rhythm at 50 bpm. The 3 abnormalities are U-waves (green arrows), failure to pace (purple box), and failure to capture (red box).
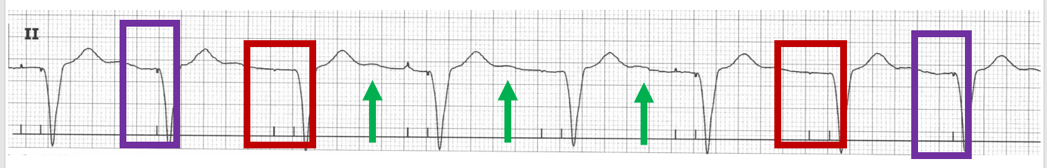
- U-waves (green arrows) are low-amplitude deflections that occurs after the T-wave, typically most visible in V2-V3 with bradycardic rates. U-waves can be seen with hypokalemia, and this patient’s potassium was 2.2 mEq/L likely due to a recent increase in her furosemide dose.
- Failure to Pace (purple boxes) describes the absence of pacer spikes when expected. Note that there are 2 pacers spikes for all the beats except for the 2 highlighted in blue boxes. The 2 pacer spikes represent the expected pacing seen with a dual chamber pacemaker: atrial pacing followed by ventricular pacing. The absence of the atrial pacing spikes in the purple boxes is likely due to the U-waves, which the pacer is mistaking for intrinsic P-waves. This was confirmed when there were no more episodes of failure to pace after the patient’s hypokalemia was treated and the U-waves disappeared.
- Failure to Capture (red boxes) describes the absence of myocardial depolarization after a pacing stimulus. Note that there is no P-wave after the initial (atrial) pacer spike in most of the beats. This also resolved after the patient’s hypokalemia was corrected, and electrolyte abnormalities are a common cause along with ischemia and structural problems (eg, wire fracture).
Learning Points
Failure to Pace
General Features
▪ Paced stimulus is not generated when expected
EKG Features
▪ Decreased or absent pacemaker function
Clinical Significance
▪ Causes: oversensing, lead fracture, or insulation defect
Oversensing: pacing inhibited by non-cardiac activity (eg, skeletal muscle activity) inappropriately recognized as native cardiac activity
Failure to Capture
General Features
▪ Delivery of pacing stimulus without subsequent myocardial depolarization
EKG Features
▪ Absence of depolarization after pacing spikes
Clinical Significance
▪ Causes: functional (electrode displacement, wire fracture) and pathologic (electrolyte disturbances, MI)
U-waves
EKG Features
▪ Low-amplitude deflection that occurs after the T-wave
▪ Most evident in V2 and/or V3
▪ Amplitude is rate dependent
- Increases with bradycardia
- Rarely seen with tachycardic heart rates
Clinical Significance
▪ Clinical significance not fully understood
▪ Can see U-wave larger than T-wave with moderate to severe hypokalemia
▪ Inverted U-waves in leads V2-V5 is abnormal (seen in ischemia and hypertension)
▪ When measuring QT, exclude U-waves or measure in a lead without U-waves (usually aVR or aVL)
Hypokalemia
General Features
▪ EKG triad of decreased T-wave amplitude, ST depression, and U-waves
EKG Features
▪ Decrease in T-wave amplitude seen first
▪ ST depressions ≥ 0.5 mm
▪ U-wave > T-wave amplitude in same lead
Clinical Significance
▪ Hypokalemia changes can be masked by tachycardia
▪ Concurrent hypomagnesemia can precipitate ventricular dysrhythmias
▪ Hypokalemia in MI is associated with increased risk of ventricular dysrhythmias
Case Conclusion
The patient was admitted to the Cardiac Short Stay Unit for electrolyte repletion, rehydration, and adjustment of her diuretic dose. Both her symptoms and her EKG abnormalities resolved with treatment, and she was discharged the next day.
For more details about pacemaker malfunctions, see Pacemaker Basics for the Emergency Physician.



