CASE
A 64-year-old male with past medical history of HTN, CAD, and prior MI presents due to substernal chest pain. What is your interpretation of his ECG?
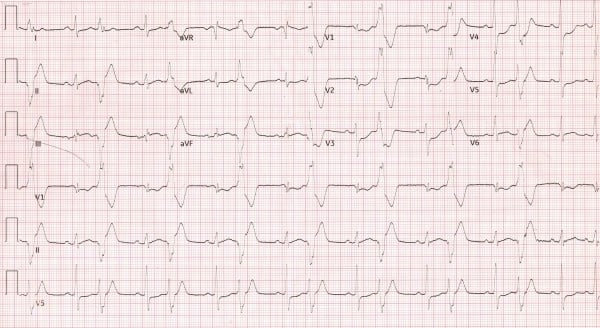
Figure 1: Case EKG
ANSWER
This ECG shows sinus rhythm with a ventricular rate of 96 in a pattern of ventricular bigeminy. In the sinus (ie, narrow complex) beats, there is STE in lead III with STD in leads I, aVL, and V1-V5. These findings are consistent with a posterior, and likely concurrent inferior, MI that warrants emergent cardiac catheterization.
Discussion
Although the STE in lead III with reciprocal STD in leads I and aVL is concerning for an impending/developing inferior MI, these findings do not meet traditional STEMI criteria. Another abnormal finding is the obliquely straight ST-segment and T-wave upstroke seen in leads II and aVF. This morphology is called the checkmark sign1 or R-T sign, and it suggests MI if new from prior, seen in contiguous leads (especially if there are reciprocal STD), and the patient’s presentation is concerning for ACS.
The STD in leads V1-V3 are consistent with a posterior MI. Prior to 2022, the ACC guidelines mandated use of a posterior ECG to diagnose a posterior MI, but this changed with the 2022 ACC Guidelines, which now recognize the following criteria as an indication for immediate angiography:2
- Horizontal STD in leads V1-V3
- Dominant R-wave (R/S ratio >1) in lead V2
- Upright T-waves in anterior leads
- Prominent and broad R-wave (>30 msec)
The 2022 guidelines also state that a posterior MI can be confirmed with a posterior ECG, but this is not mandated as a criterion for emergent cardiac catheterization.
This case occurred prior to the 2022 guidelines, so a repeat ECG with posterior leads was obtained (see Figure 2). The repeat ECG shows STE in leads II, III, and aVF, with STD in leads I and aVL that meet STEMI criteria and underscore the importance of obtaining serial ECGs in patients with an equivocal initial ECG and a presentation concerning for ACS. This ECG also shows STE in leads V7-V9, diagnostic of a posterior MI.

Figure 2: Posterior ECG
The diagnostic criteria for a posterior MI2 differ from traditional STEMI criteria in 2 important ways:
- There only needs to be STE in 1 posterior lead
- The STE only needs to be ≥ 0.5 mm
Another change in the 2022 ACC guidelines is the removal of the STE cutoff of ≥ 1 mm for men < 40 years old. Placement of posterior leads is described in the Learning Points below.
Posterior MIs are typically seen with a concurrent inferior or lateral MI, but an estimated 5-10% of MIs are isolated posterior MI. The blood supply for the posterior wall is supplied by the posterior descending artery which can be supplied by the RCA (~80% of the population), the LCx (~10% of the population), or by both the RCA and LCx (~10% of the population). These anatomic configurations are referred to as right dominant, left dominant, and co-dominant circulation, respectively. Isolated posterior MI are commonly missed because they don’t manifest STE on a traditional 12-lead ECG and may only manifest subtle STE on a posterior ECG. Accordingly, it is important not to misdiagnose STD in leads V1-V4 as anteroseptal ischemia and miss an isolated posterior MI that warrants emergent cardiac catheterization.
Case Conclusion
This patient was taken to the catheterization laboratory, where a 100% occlusion of the left circumflex artery was successfully stented.
Posterior MI Learning Points
- Consider whenever there is STD in leads V1-V4, especially if there are concurrent prominent R-waves and/or upright T-waves in these leads
- Use posterior leads V7-V9 (see Figure 3) to evaluate for posterior MI if there is diagnostic uncertainty regarding STD in leads V1-V4
- V7- left posterior axillary line at the 5th intercostal space
- V8- left midscapular line at the 5th intercostal space
- V9- left paraspinal border at the 5th intercostal space
- STE ≥ 0.5 mm in posterior leads V7, V8, or V9 is diagnostic
- Does not require 2 contiguous leads
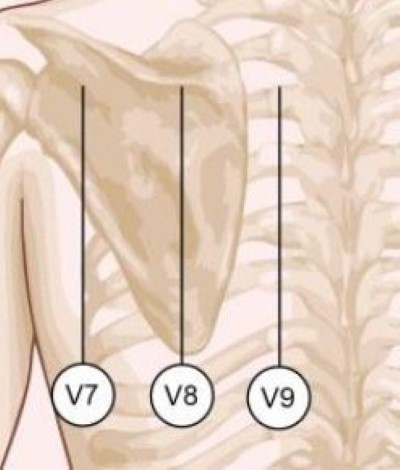
Figure 3: Posterior lead placement
Disclaimer: Dr. Good and Dr. Regino are employed by HCA Healthcare and/or an HCA Healthcare-affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
References
- Mattu A. ECGWeekly.com.
- Kontos M, de Lemos J, et al. 2022 ACC Expert Consensus Decision Pathway on the Evaluation and Disposition of Acute Chest Pain in the Emergency Department. J Am Coll Cardiol. 2022;80(20):1925–1960.
- Oraii S, Maleki M, Abbas Tavakolian A, et al. Prevalence and outcome of ST-segment elevation in posterior electrocardiographic leads during acute myocardial infarction. J Electrocardiol. 1999;32(3):275-278.



