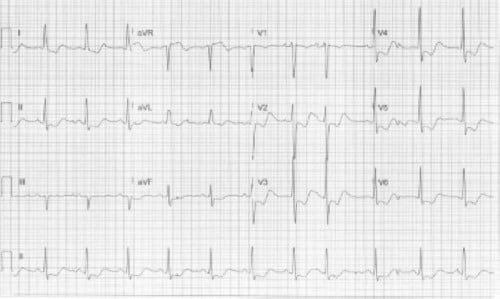
A 58-year-old male with a PMH of alcohol use disorder presents to the ED due to multiple falls. What is your interpretation of his ECG?
Answer
This ECG shows normal sinus rhythm at 70 bpm, normal axis, prolonged QRS complex duration with an IVCD, prolonged QTc interval, and STE in lead aVR. There are also STD, TWI, and U-waves in leads I, II, and V2-V6, all of which are seen with hypokalemia.
Potassium is primarily an intracellular ion and is critical in maintaining the resting membrane potential of the myocardium and is crucial during phases 2 and 3 of the cardiac action potential (AP). Hypokalemia leads to an increased risk of early afterdepolarizations (EADs) which are defined as a slowing or reversal of the normal repolarization during phase 2 or 3 of the cardiac AP. These EADs can trigger ventricular dysrhythmias such as torsades de pointes, polymorphic VT, and ventricular fibrillation.
The classic ECG finding seen in hypokalemia is the U-wave which is defined as a positive deflection after the T-wave, best seen in the anterior precordial leads at slower heart rates. U-waves are not specific for hypokalemia and can be due to hypomagnesemia, hypercalcemia, hypothermia, LVH, and medications. Other ECG findings in hypokalemia include increased amplitude and duration of the P-wave and QRS complex and PR interval prolongation.
The classic triad of ECG changes associated with hypokalemia includes TWI, STD, and U-waves, but all three findings are not always present, even with severe hypokalemia. When all three findings are present, it creates a “reverse Wellens” pattern of a downward deflection followed by an upward deflection following the QRS complex as seen in the case ECG. This pattern also resembles the graph of y=-sin(x) (see Figure 1), so the authors propose calling this the “negative sine sign”. [Editor’s note: Dr. Schenker would like the readers to know that he had nothing to do with this and vehemently opposes the use of trigonometry in ECG education.]
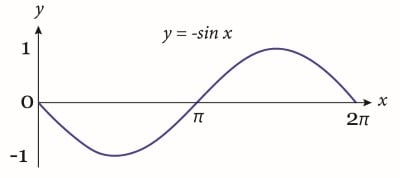
Figure 1. The “negative sine sign”
There is controversy regrading whether hypokalemia truly causes a prolonged QT interval or just the appearance of a prolonged QT interval due to the presence of U-waves (i.e., should the U-wave be included when measuring the QT interval). Regardless, hypokalemia that produces the appearance of a prolonged QT interval, TU complexes, or significant U-waves, increases the risk for ventricular dysrhythmias, in particular torsade de pointes.
The challenging aspect of treating hypokalemia-induced ventricular dysrhythmias is knowing how much potassium can be administered emergently and how quickly can it be given. Institutional protocols typically limit potassium replacement to 10 mEq/hour via peripheral access and 20 mEq/hour via central access, both of which may be insufficient to stabilize a patient with a ventricular dysrhythmia due to severe hypokalemia. The 2000 AHA ACLS guidelines state “If cardiac arrest from hypokalemia is imminent (ie, malignant ventricular arrhythmias), rapid replacement of potassium is required. Give an initial infusion of 2 mEq/min, followed by another 10 mEq IV over 5 to 10 minutes… Once the patient is stabilized, reduce the infusion to continue potassium replacement more gradually.”1 The 2005 AHA CPR guidelines state, “If cardiac arrest from hypokalemia is imminent (i.e., malignant ventricular arrhythmias are present), rapid replacement of potassium is required. Give an initial infusion of 10 mEq IV over 5 minutes; repeat once if needed.”2
Case Conclusion
This patient’s workup was notable for a serum potassium level of 1.7 mEq/L. He was treated with IV and oral potassium and admitted to the internal medicine service.
Hypokalemia Learning Points
General Features:
- ECG triad of decreased TWI, STD, and U-waves (the “negative sine sign”)
EKG Features:
- T-wave flattening or inversion
- U-waves
- Slight STD
- STE in aVR
- Increased P-wave and QRS complex amplitude and duration
- PR interval prolongation
- QTc prolongation
- Increased ectopy (e.g., premature beats) and tachydysrhythmias
Clinical Significance:
- Hypokalemia changes can be masked by tachycardia
- Concurrent hypomagnesemia can precipitate ventricular dysrhythmias
- Prolonged QTc = increased risk of torsades de pointes
References
- ECG Guideline, Part 8: Advanced Challenges in Resuscitation Section 1: Life-Threatening Electrolyte Abnormalities, Circulation Volume 102, Issue suppl_1, 22 August 2000; Pages I-217-I-222
- 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, Part 10.1: Life-Threatening Electrolyte Abnormalities. Originally published28 Nov2005 https://doi.org/10.1161/CIRCULATIONAHA.105.166563Circulation. 2005;112:IV-121–IV-125



