A 33-year-old male presents to the emergency department because of palpitations. He reports a history of similar episodes in the past that always respond to adenosine. What is your interpretation of the ECG?
Answer
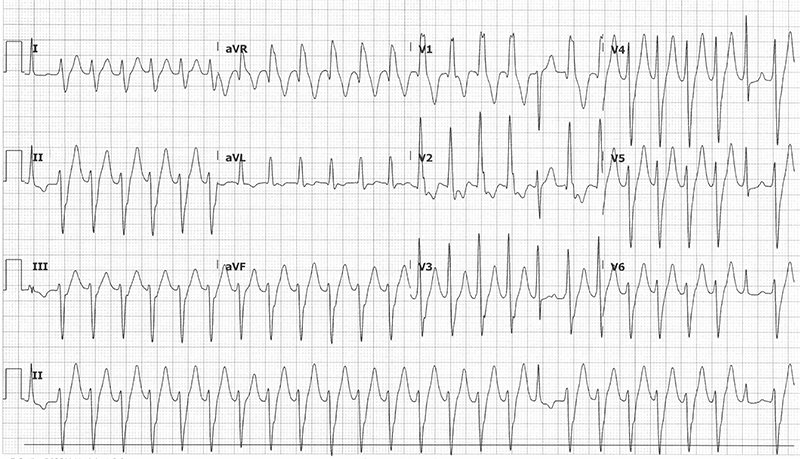
This ECG shows a regular wide complex tachycardia with a ventricular rate of 155 bpm, no visible P-waves, northwest/extreme axis deviation, prolonged QRS duration of 130 ms with a RBBB morphology, ST-segment and T-wave discordance, and 3 narrow complex beats.
The differential for a regular WCT includes:
- Monomorphic ventricular tachycardia
- SVT with aberrant conduction
- Antidromic SVT (WPW)
- Any SVT (sinus tach, AVNRT, atrial flutter, etc.) with fixed or rate-related BBB
- Any SVT with metabolic abnormalities
- Any SVT with sodium channel blocking toxicity
The key to interpreting this ECG is beats 1, 18, and 25. These narrow complex beats are suggestive of capture and fusion beats, which are considered pathognomonic for ventricular tachycardia.
This patient was known to have idiopathic fascicular ventricular tachycardia (IFVT), also called verapamil-sensitive VT. In this patient’s case, the VT does break with adenosine, but this variant of VT does not reliably respond to adenosine.
Basics of VT
Ventricular tachycardia is defined as a cardiac arrhythmia of ≥ 3 consecutive beats that originate in the ventricle with a wide QRS complex ≥ 120 ms at a rate >100. Sustained VT is defined as lasting ≥ 30 seconds or causing hemodynamic collapse regardless of duration. Non-sustained VT is defined as lasting < 30 seconds with no hemodynamic compromise. VT can be further categorized into monomorphic and polymorphic. Risk factors include structural heart disease and scar tissue from prior ischemia/infarct.
ECG findings that are considered pathognomonic for VT include AV dissociation, fusions beats, and capture beats. A fusion beat is a complex between a supraventricular impulse that originates above the AV node which fuses with an impulse generated in the ventricle (red box marked with F in Figure 1). Capture beats happen when a supraventricular impulse conduct normally through the AV node amid AV dissociation (blue boxes marked with C in Figure 1).
Figure 1. ECG Findings in VT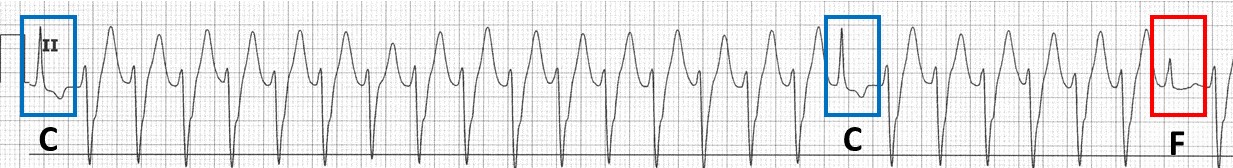
Management of VT
Always start with the ABCs, ensure you have adequate IV access, place the patient on a continuous ECG monitor, and place your cardiac pads in the anterior/posterior positioning.
Treatment options for stable patients include:
- Amiodarone 150 mg over 10 min followed by a drip at 1 mg/min for 6 hrs
- Lidocaine 1–1.5 mg/kg
- Procainamide 20–50 mg/min until VT terminates, or a max dose of 17 mg/kg
Treatment options for unstable patients include:
- Synchronized cardioversion at 100 J with increasing energy for each subsequent shock (note that this is also an option for stable patients)
Idiopathic Fascicular Ventricular Tachycardia
Idiopathic ventricular tachycardias represent ~10% of all ventricular tachycardias, arise spontaneously in the absence of structural heart disease, and are generally seen in young, healthy patients. ~10-15% of idiopathic VTs occur in the left ventricular conduction system, called idiopathic fascicular ventricular tachycardia, with the remainder occurring in the right ventricle.
Idiopathic fascicular ventricular tachycardia (IFVT), also known as verapamil-sensitive VT, idiopathic left ventricular tachycardia, and Belhassen VT, is a re-entry tachycardia from an ectopic focus in the left ventricular conduction system. The ECG will show a RBBB pattern with a relatively mild prolongation of the QRS interval (120-140 ms), as seen in this patient’s ECG, when compared to other VTs.
IFVT can easily be confused with supraventricular tachycardias with aberrant conduction, however the presence of capture beats, fusion beats, or AV dissociations can help distinguish IFVT from SVT. Unlike SVT, adenosine and vagal maneuvers are not reliably effective in treating IFVT. Additionally, unlike traditional ventricular tachycardias, Class I antiarrhythmics such as lidocaine and procainamide are also not effective. As the name verapamil-sensitive VT suggests, this rhythm is very responsive to verapamil at a dose of 2.5–5 mg given IV every 15–30 minutes.
Case Conclusion
This patient was known to have IFVT diagnosed on prior EP studies. He was treated with adenosine, which terminated the VT. In this patient’s case, the VT did break with adenosine, but it important to recognize that this variant of VT does not reliably respond to adenosine.
Learning Points
Monomorphic VT
- ≥ 3 consecutive, regular, wide complex beats with rate > 100
- Non-sustained: < 30 sec duration with no hemodynamic instability
- Sustained: ≥ 30 sec duration OR causes hemodynamic instability
ECG features that increase the likelihood of VT in a WCT:
- QRS > 200 ms is almost always VT or hyperkalemia with aberrancy
- AV dissociation (ventricular rate > atrial rate)
- Positive or negative QRS concordance in leads V1-V6 (entirely or predominantly positive or negative QRS complexes from V1 to V6)
- Extreme axis deviation (“northwest axis”)
- If BBB pattern is present, the absence of typical RBBB or LBBB pattern suggests VT (ie, normal RBBB or LBBB pattern makes SVT with aberrant conduction more likely)
- Fusion beats- hybrid QRS complex formed by fusion of a supraventricular impulse and ventricular impulse
- Capture beats- sinus QRS formed by transient normal conduction amid AV dissociation
- Brugada’s sign- time from the onset of the QRS complex to the nadir of the S-wave is > 100 ms
- Josephson’s sign- notching near the nadir of the S-wave



