With the wide-ranging presentations seen among COVID-19 patients, it can be easy to miss other conditions.
May 2020: You are a resident in a busy inner-city ED in the trenches of the coronavirus pandemic. You get an ALS call: 44-year-old male with no known past medical history coming in for shortness of breath, reportedly saturating 80% on room air. It seems you have heard this history thousands of times by now, and your next steps have become rote. The escalation algorithm flashes in your head: nasal cannula, non-rebreather mask, non-invasive positive pressure ventilation, and, if all else fails, endotracheal intubation.
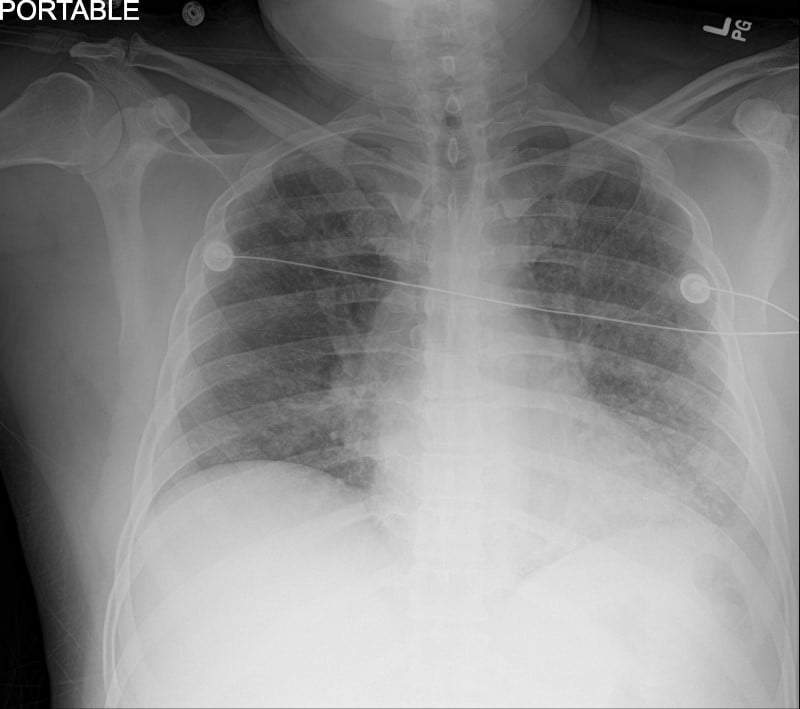
The patient arrives in moderate respiratory distress, tachypneic, with a respiratory rate > 40. There is obvious increased work of breathing, though he is still able to speak in full sentences. He has had some tactile fevers and gastrointestinal symptoms as well, both of which you know by now are typical for novel coronavirus. The patient goes on to explain that his wife and daughter have similar symptoms and are also patients in the ED, further solidifying a viral picture in your head. Treatment with oxygen via nonrebreather improves his symptoms. You establish IV access, get labs, and continue to monitor the patient. Chest radiography looks familiar: bilateral ground glass opacities (Figure 1).
Arterial blood gas reveals a P/F (PaO2/FiO2) ratio of 116. The lab work comes back to show moderately high leukocytosis – not something routinely associated with COVID-19, but it seems there is something new every day with this virus, forcing diagnostic flexibility.
Then you notice something else odd: his inflammatory markers (namely D-Dimer and ferritin) are not as elevated as you have come to expect. Your perplexity increases when the COVID-19 nasopharyngeal swab testing comes back negative. Are you missing something here?
Upon re-evaluation, the patient mentions that during his time in quarantine he decided to clean out his home aquarium for the first time in seven years. He didn't use any chemicals, but his aquarium contains some living coral over which he ran hot water. Could this be related to the clinical presentation?
Discussion
Palytoxin is a nonprotein environmental toxin found in coral species: specifically, species of Zoanthid coral, which include the Palythoa and Zoanthus subspecies. This compound was first isolated in the 1970s and is thought to be one of the most toxic marine substances ever classified.1 The ornate corals that contain this toxin are soft; they are occasionally used in home aquariums and in some places are available for commercial purchase. In vivo, palytoxin acts on blood vessels to cause vasoconstriction. On the cellular level palytoxin inhibits the sodium-potassium ATPase.2
Though exceedingly rare, inhalation can cause respiratory distress and even respiratory failure. The irritant properties of palytoxin are postulated to contribute to the inflammatory reactions seen with inhalational contact.3 Often released upon cleaning this specific type of coral, steam containing palytoxin has been described by those exposed as pungent and foul smelling. Symptom onset is usually minutes to hours following exposure.4-7 Laboratory studies often show leukocytosis and patients can present febrile as well.8 Without sufficient history, this presentation could easily be mistaken for pneumonia, especially in conjunction with an abnormal chest x-ray, as seen in this and other cases.9-10
Aside from respiratory distress and failure, in some reports, clinical toxidrome can present with gastrointestinal symptoms and distorted sense of taste,1 very similar to the presentation of the 2019 novel coronavirus. Palytoxin may even cause generalized fatigue and muscle weakness due to rhabdomyolysis or cardiac dysrhythmias,10 and overall can lead to death.1,11
In addition to inhalation exposure, there are also reports of gastrointestinal as well as dermatological related toxicity through ingesting the toxin in contaminated seafood or handling coral, respectively.4-5 There is no specific antitoxin for this entity. Treatment is often supportive, sometimes including inhaled steroids. Patients usually recover within several days of exposure.
Case Conclusion
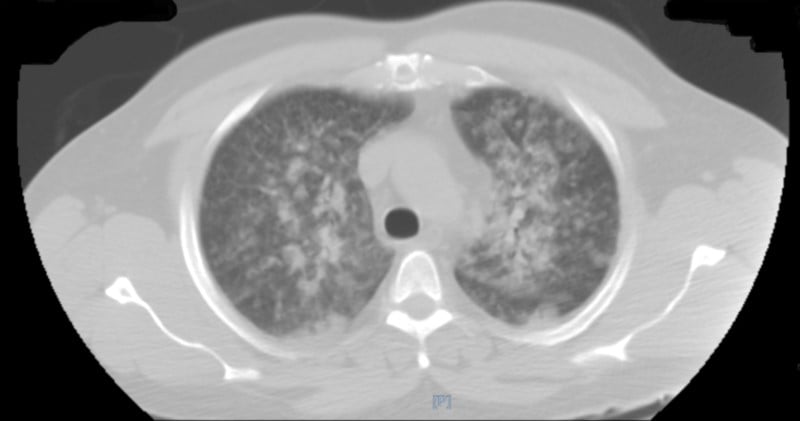
The patient, his wife, and daughter were all admitted to the hospital. The patient and wife were afebrile on presentation; however, their daughter had a temperature of 101°F. Labs showed elevated ESR, CRP, lactic acid, and procalcitonin, as well as acute kidney injury. The patient had a CT of the chest that showed confluent ground-glass opacities with areas of consolidation involving the lung apices, as well as interlobular septal thickening (Figure 2).
Leukocytosis (white blood cell counts as high as 27 x 103/uL for the patient, 35 for the wife, and 37 for his daughter) trended down over time. Each family member stayed in the hospital for several days, with symptoms and chest x-ray infiltrates peaking on day 2 - 3. High flow nasal cannula was used for symptomatic treatment for all three and the patient's acute kidney injury resolved with hydration. The family was discharged with strict instructions not to handle or attempt to clean the coral again.
References
- Vick JA, Wiles JS. The mechanism of action and treatment of palytoxin poisoning. Toxicol Appl Pharmacol. 1975;34(2):214-223.
- Freilin C, Breittmayer JP. Palytoxin: Mechanism of Acidifying Action in Excitable Cells. Methods in Neurosciences: Neurotoxins. Edition 8. San Diego, CA. Academic Press. 347-357.
- Tubaro A, Durando P, Del Favero G, Ansaldi F, Icardi G, Deeds JR, Sosa S. Case definitions for human poisonings postulated to palytoxins exposure. Toxicon. 2011;57(3)478-495.
- Sud P, Su MK, Greller HA, Majlesi N, Gupta A. Case series: inhaled coral vapor toxicity in a tank. J Med Toxicol. 2013;9(3):282-286.
- Hamade AK, Deglin SE, McLaughlin JB, Deeds JR, Handy SM, Knolhoff AM. Suspected Palytoxin Inhalation Exposures Associated with Zoanthid Corals in Aquarium Shops and Homes - Alaska, 2012-2014. MMWR Morb Mortal Wkly Rep. 2015;64(31):852-855.
- Schulz M, Łoś A, Szabelak A, Strachecka A. Inhalation poisoning with palytoxin from aquarium coral: case description and safety advice. Arh Hig Rada Toksikol. 2019;70(1):14-17.
- Thakur LK, Jha KK. Palytoxin-induced acute respiratory failure. Respir Med Case Rep. 2017;20:4-6.
- Snoeks K, Veenstra J. Family with fever after cleaning a sea aquarium. Ned Tijdschr Geneeskd. 2012;156(12):A4200.
- Hall C, Levy D, Sattler S. A Case of Palytoxin Poisoning in a Home Aquarium Enthusiast and His Family. Case Rep Emerg Med. 2015.
- Deeds R, Schwartz MD. Human risk associated with palytoxin exposure. Toxicon. 2010;56(2):150-162.
- Riobó and J. M. Franco. Palytoxins: biological and chemical determination. Toxicon. 2011;57(3):368-375.



