BRASH syndrome is an uncommon but often fatal condition in which an acute renal injury initiates a vicious cycle of bradycardia, hyperkalemia, hypotension and worsening renal failure in patients who take AV-nodal blocking medications.
We report a case of an 84-year-old male taking an AV-nodal blocker (amlodipine) who presented in acute renal failure with profound bradycardia and slight hyperkalemia. He had minimal symptoms and was well-appearing at presentation; however, his condition rapidly deteriorated and he died the next day. The final diagnosis was BRASH syndrome.
Case
An 84-year-old male presented to the emergency department via EMS from his long-term care facility after staff became concerned that he was “lethargic.” EMS noted a heart rate of 23 bpm and administered a 1L NS bolus without improvement in heart rate. Upon arrival to the ED, the patient was sitting up in a position of comfort, interacting with staff, answering questions appropriately, moving all extremities equally and appeared well and nontoxic. Vital signs were remarkable for HR 31 bpm, BP118/50, RR 18 rpm, O2 saturation of 89% on room air. He was afebrile. There were no remarkable physical exam findings aside from bradycardia with a systolic murmur. The only symptoms the patient reported were an episode of thoracic back and bilateral shoulder pain the night before presentation and one episode of dark stools the week prior. His past medical history was significant for hypertension, congestive heart failure, chronic kidney disease, and former tobacco use. His medications included amlodipine 10 mg daily, hydralazine 25 mg three times daily, atorvastatin 20 mg daily, furosemide 20 mg daily, and aspirin 81 mg daily.
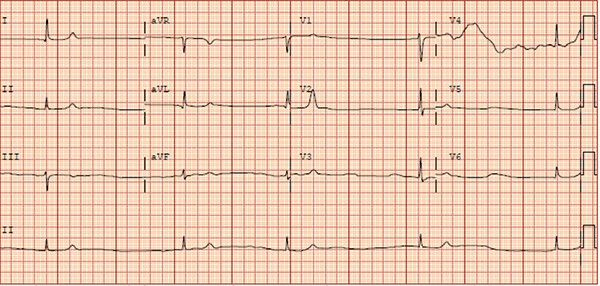
EKG obtained on arrival demonstrated severe junctional bradycardia with a heart rate of 27 bpm (Figure 1). A broad workup included: CBC, BMP, BNP, high-sensitivity troponin, PT/PTT/INR, TSH, magnesium level, ionized calcium level, and CXR. The patient was found to be in acute renal failure, with a creatinine of 7.9 mg/dL. Potassium was slightly elevated to 5.8 mmol/L. Troponin and BNP were within range of the patient’s baseline. Hemoglobin was low at 7.6 g/dL, but was within the patient’s baseline. Chest x-ray demonstrated pulmonary vascular congestion and slight interstitial edema, which was thought to be the etiology of his mild hypoxia in the setting of known CHF history.
Figure 1. Initial EKG demonstrates junctional rhythm with severe bradycardia
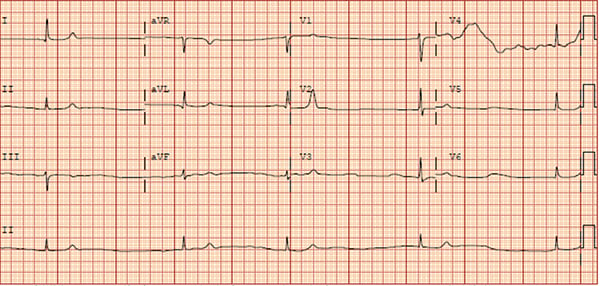
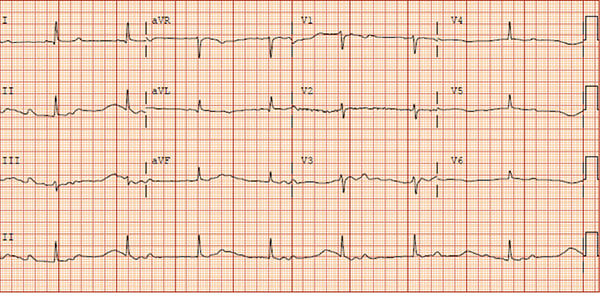
Cardiology was consulted early in the ED course and the patient was given atropine, which brought his heart rate up to 46 bpm from 31 bpm (Figure 2). He was admitted to the ICU with the goal of improving renal function prior to placing a pacemaker. His ICU stay was notable for persistent bradycardia as low as 28 bpm, which was not responsive to continuous dopamine infusion. As his condition deteriorated, he was not deemed to be a candidate for pacemaker placement or hemodialysis and the family ultimately decided to transition to comfort care. An inciting event for the acute renal injury was not clearly identified but was thought to be cardio-renal syndrome.
Figure 2. Repeat EKG after atropine; increased HR (though still bradycardic) with morphology unchanged
Discussion
BRASH Syndrome is a fairly new entity that was formally recognized as a distinct disease process in 2016.1 The acronym stands for: Bradycardia, Renal failure, AV-nodal blockade, Shock, and Hyperkalemia. The proposed pathophysiology centers on a cycle of hypoperfusion and bradycardia instigated by AV-nodal blockade and hyperkalemia.
BRASH Syndrome occurs in patients taking an AV-nodal blocking agent (commonly beta-blockers or calcium-channel blockers) who subsequently develop acute renal injury.1 As the renal injury progresses, patients become hyperkalemic and the AV-nodal blocking agent begins to accumulate.1 These two factors, hyperkalemia and AV-nodal blockade, act synergistically to cause bradycardia and hypotension.1,2 This leads to end organ hypoperfusion, which further worsens renal function.1 And the vicious cycle continues. The presence of an angiotensin converting enzyme inhibitor or angiotension II receptor blocker medication, which can also cause potassium retention and decrease GFR, potentiates the cycle.1
The typical patient will be an elderly individual who clinically appears much better than expected for the degree of bradycardia.1 However, patient presentations do range from asymptomatic to obtunded with multi-system organ failure.1 The inciting event causing poor renal function may be dehydration from poor oral intake, increased output from illness such as enteritis, or any other cause of renal injury.
The diagnosis of BRASH syndrome is complicated by the fact that patients often appear well with minimal symptoms and labs are often not particularly striking. BRASH syndrome patients often have only mild hyperkalemia (5.5-6.0 mmol/L) as opposed to the very high levels needed in pure hyperkalemia required to cause the same degree of bradycardia seen in BRASH syndrome.1 This is due to the synergistic effects of mild hyperkalemia and AV-nodal blockade.1 Similarly, EKG findings in BRASH syndrome typically show significant bradycardia without the classic stigmata of hyperkalemia (eg, peaked T waves, sine waves, etc.).1,3 Lastly, patients with BRASH syndrome are typically adherent to proper medication dosing and rarely have supra-therapeutic blood levels of AV-nodal blocking agents.1,4
Treatment in the ED
The treatment of BRASH Syndrome prioritizes reduction of hyperkalemia, increasing heart rate, and addressing the underlying cause of acute kidney injury.4,5,6 Standard treatment for hyperkalemia should be employed quickly, including IV calcium to stabilize the cardiac membrane, insulin with dextrose drips, high-dose albuterol, and bicarbonate to drive potassium into cells, as well as diuretics to expel potassium from the body.1,4,5,6,7 Calcium and albuterol have the added benefit of improving heart rate in these bradycardic patients. For those with profound bradycardia, epinephrine (first-line) or isoproterenol (second-line) can be used to increase heart rate if the patient is also hypotensive, otherwise dobutamine can be used if normotensive.1,4,5,6,7 Of note, atropine is often ineffective as it works at the AV node, which is blocked by the beta-blockers and calcium-channel blockers that instigate BRASH syndrome.4,5 Transcutaneous or transvenous pacing may be necessary, and at least two case reports document pacemaker placement.1 Reestablishing adequate kidney perfusion is paramount, as this helps eliminate potassium from the body through kaliuresis and breaks the cycle of BRASH syndrome.1,4,5,6 This can be achieved by fluid resuscitation, especially given patients are often dehydrated, and pressor support if profoundly ill.4,6
The precise prevalence of BRASH Syndrome remains unknown.5 However, if a physician encounters a patient with bradycardia on an AV-nodal blocking agent who does not respond to the standard ACLS guidelines for treatment of bradycardia, BRASH Syndrome should be considered.6 Although a rare condition, BRASH Syndrome can be lethal when not properly addressed. Therefore, it is essential to keep BRASH Syndrome in the differential diagnosis.
TAKE-HOME POINTS
- BRASH Syndrome is a constellation of Bradycardia, Renal failure, AV-nodal blockade, Shock, and H
- BRASH Syndrome is commonly triggered by an acute event (ie, dehydration) that results in kidney injury and hyperkalemia.
- Potassium levels in BRASH Syndrome are often only mildly elevated but act synergistically with AV-nodal blockade agents to cause hypotension and bradycardia.
- Treatment involves lowering potassium levels, improving renal function by treating the underlying cause, and increasing heart rate; however, atropine is often ineffective.
References
- Farkas JD, Long B, Koyfman A, Menson K. BRASH Syndrome: Bradycardia, Renal Failure, AV Blockade, Shock, and Hyperkalemia. The Journal of Emergency Medicine. 2020; 59(2):216-223. https://www.sciencedirect.com/science/article/pii/S0736467920303991. Accessed January 22, 2021.
- Hegazi MO, Aldabie G, Al-Mutairi S, El Sayed A. Junctional bradycardia with verapamil in renal failure--care required even with mild hyperkalaemia. Journal of clinical pharmacy and therapeutics. 2012; 37(6):726-728. https://pubmed.ncbi.nlm.nih.gov/22568727/. Accessed January 22, 2021.
- Lee TH, Salomon DR, Rayment CM, Antman EM. Hypotension and sinus arrest with exercise-induced hyperkalemia and combined verapamil/propranolol therapy. The American journal of medicine. 1986; 80(6):1203-1204 https://pubmed.ncbi.nlm.nih.gov/3728515/. Accessed January 22, 2021.
- Farkas J. PulmCrit- BRASH syndrome: Bradycardia, Renal failure, Av blocker, Shock, Hyperkalemia. EMCrit Project. 2016. https://emcrit.org/pulmcrit/brash-syndrome-bradycardia-renal-failure-av-blocker-shock-hyperkalemia/. Accessed January 22, 2021.
- Farkas J. BRASH syndrome. EMCrit Project. 2020. https://emcrit.org/ibcc/brash/. Accessed January 28, 2021.
- Prabhu V, Hsu E, Lestin S, Soltanianzadeh Y, Hadi S. Bradycardia, Renal Failure, Atrioventricular Nodal Blockade, Shock, and Hyperkalemia (BRASH) Syndrome as a Presentation of Coronavirus Disease 2019. Cureus, 2020;12(4):e7816. doi:10.7759/cureus.7816. Accessed January 14, 2021.
- Dépret F, Peacock WF, Liu KD, Rafique Z, Rossignol P, Legrand M: Management of hyperkalemia in the acutely ill patient. Ann Intensive Care. 9(32). https://annalsofintensivecare.springeropen.com/articles/10.1186/s13613-019-0509-8. Accessed February 14, 2021.