The HEART score is a go-to tool in assessing the risk of an acute coronary syndrome. But in this case, a score of 3 did not mean the 29-year-old patient was safe.
Cardiovascular disease (CVD) is currently the leading cause of death in both men and women across the United States. The term describes a group of diseases that includes coronary artery disease, myocardial infarction (MI), stroke, and heart failure. There are both modifiable and non-modifiable risk factors that can increase the risk of a person’s susceptibility to CVD. Non-modifiable risk factors include ethnicity, family history of CVD, sex, and age. Historically, studies regarding CVD use 40-45 years old as the lower limit defining a “young” patient with CVD. These studies have found that 5-10% of patients experiencing an MI are younger than 40.1
When a patient presents to the ED with chest pain, the HEART score is often used to assess the risk of an acute coronary syndrome (ACS). The parameters of the HEART score include a suspicious history, ischemic ECG findings, age, number of cardiac risk factors, and initial troponin levels. Each category will receive a value of 0, 1, or 2 for a maximum score of 10; a patient under 45 years old receives 0 points for the age category. A patient’s total HEART score can classify their 6-week risk of a major cardiac event as low, moderate, or high. In the case below, the patient received a HEART score of 3, a low score representing 0.9-1.7%2 risk of having a major cardiac event.
CASE REPORT
A 29-year-old Caucasian male with history of acute lymphoblastic leukemia (ALL) treated with full body radiation, marrow transplant and chemotherapy 12 years ago, presents to the ER with acute chest pain and SOB that began 3.5 hours prior to arrival, while delivering food. He then walked into the local CVS to check his blood pressure, which was “150s/90s.” Although unable to describe the quality of the pain, he is writhing in pain on the stretcher and rates it a 10/10. Nothing seems to be giving him any relief. He denies any similar past episodes. The patient does is not currently on any medications, denies a history of smoking or illicit drug use. The patient’s father has a history of CAD in his 50s, and his mother’s health is unremarkable. The patient has been in complete remission from ALL for 12 years; he has no other medical conditions.
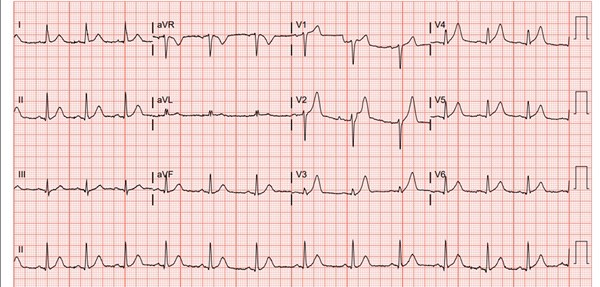
Figure 1. Initial EKG Reading
The patient’s initial workup in the ED included an ECG, chest X-ray, complete blood count, comprehensive metabolic panel, cardiac enzymes, lipase, and coagulation studies. His initial vitals were unremarkable. His initial EKG (Figure 1) performed in triage, showed normal sinus rhythm with hyperacute T wave changes in V2-V6; his potassium was 4.3. His other labs were unremarkable except for a troponin-I of 0.41.
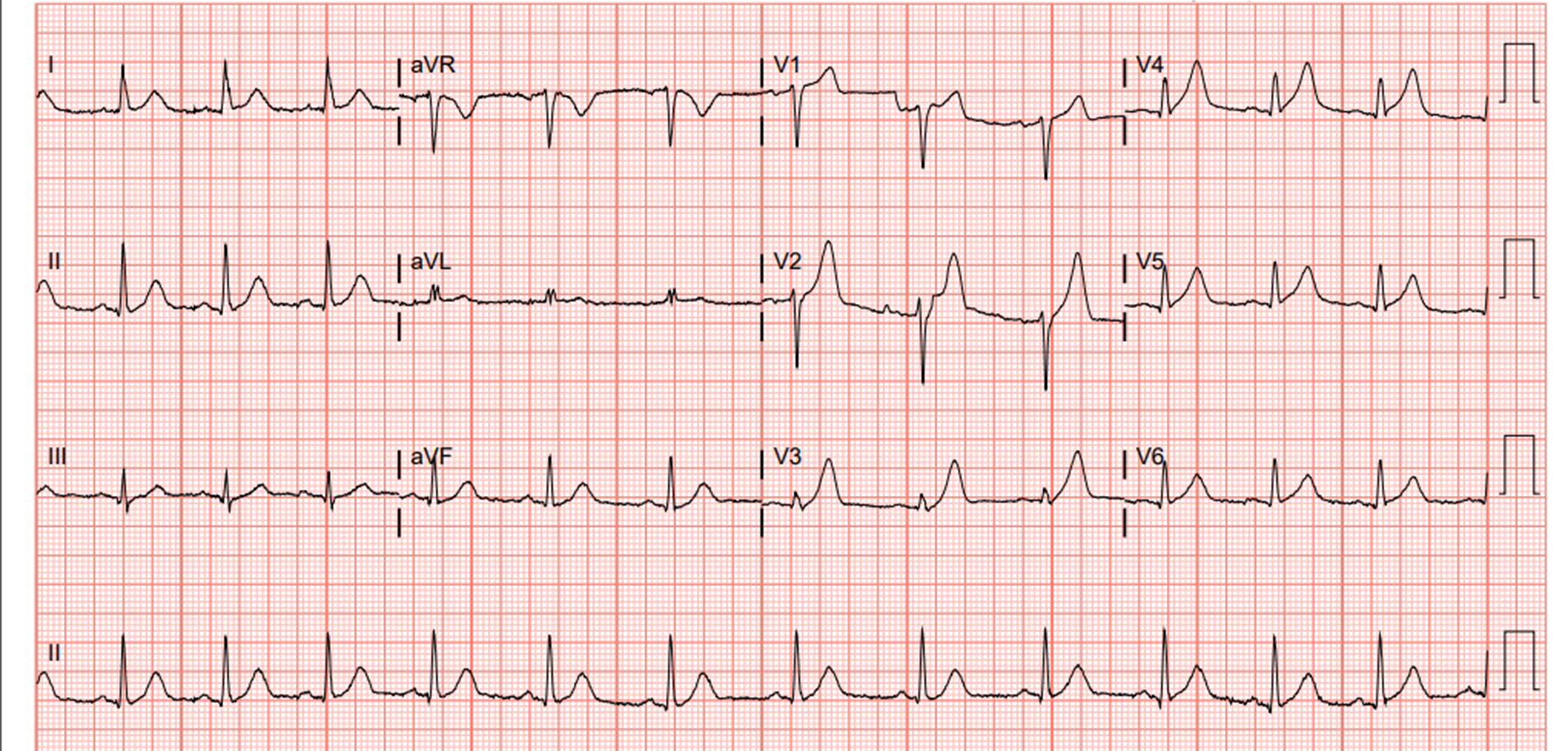
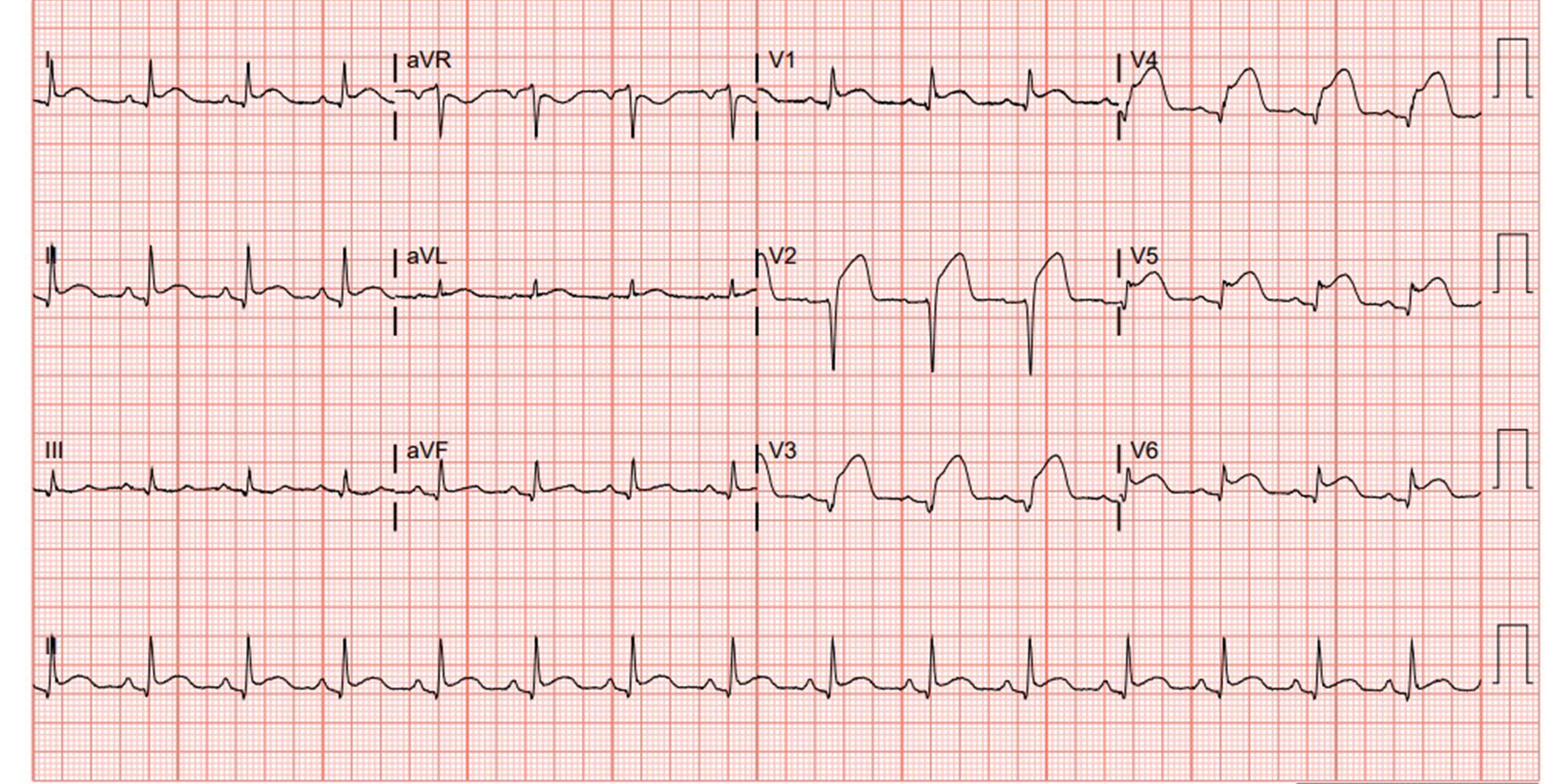
A repeat ECG (Figure 2) was obtained 1.5 hours after the first, which showed normal sinus rhythm with significant ST segment elevation in leads I, II, and V1 through V6, suggesting an anterolateral MI.
The patient was immediately given aspirin, morphine, nitroglycerin, and heparin and was taken for emergent cardiac catheterization. Upon catheterization, he was found to have a 100-percent occlusion along the middle portion of the left anterior descending (LAD) artery; no occlusions were found in the right coronary artery or the the circumflex artery.
Stents were placed along the first and second diagonal branches of the LAD. During the procedure, the patient had several episodes of ventricular tachycardia, which resolved with deep coughing, and also had an episode of ventricular fibrillation requiring cardioversion to sinus rhythm. The catheterization lab report also noted that patient had an anterolateral apical hypokinesia and a left ventricular function of 40%.
Following percutaneous coronary intervention, the patient was admitted to the intensive care unit for further monitoring.
Discussion
As a patient with low CVD risk factors, is important to consider the history of pediatric cancer. When the patient presented to the ED, he had been in complete remission from ALL for 12 years. As a child, he had undergone numerous combinations of chemotherapy, radiation, and eventually a bone marrow transplant. Studies have examined the development of atherosclerosis in patients who have received radiation.3 In pediatric cancer patients, individuals who live more than 5 years following their radiation have shown an eightfold increase in their risk of developing atherosclerosis compared to the general population later in their life.3
Another factor to consider in an ECG of a patient complaining of chest pain is the T wave. The T wave in an ECG is a reflection of the repolarization of the ventricles of the heart. The majority of T waves have a positive direction and should be asymmetric with a slow upstroke and a rapid downstroke.4 The T waves in the limb leads should be less than 5 mm, and those in the chest leads should be less than 10 mm.4 Upon the initial ECG of this patient, it was important to rule out any abnormalities in T wave presentation that could reflect underlying pathology of the heart. No evidence of hyperkalemia in the form of peaked T waves that could lead to fatal arrhythmias were seen at the time. However, hyperacute T waves were seen in leads II and V2 through V6. Hyperacute T waves are often, but not always, known to precede ST segment elevation. They are the earliest available electrical event that can be detected on an ECG during an acute ischemic event and can rapidly progress into ST segment elevation.4 While a hyperacute T wave is not always associated with ST elevation, if detected on an ECG, the emergency physician should consider ordering serial ECGs along with the cardiac biomarkers to look out for any acute cardiac event.
References
1. Azar RR. Coronary heart disease and myocardial infarction in young men and women. UptoDate. Accessed November 6, 2018.
2. Wilson PWF. Cardiovascular disease risk assessment for primary prevention: Risk calculators. UpToDate. Accessed November 6, 2018.
3. Haddy N, Diallo S, El-Fayech C, et al. Cardiac Diseases Following Childhood Cancer Treatment. Circulation. 2016;133(1):31-38.
4. Prutkin JM. ECG Tutorial: ST and T wave changes. UpToDate. Accessed November 6, 2018.