The Med Student Quick Guide for Reading EKGs
Allison Gasnick, MS4
Case Western Reserve University School of Medicine
Editor, Medical Student Council 2024
This is not meant to be an exhaustive guide. EKG interpretation is nuanced and takes years of training to master. There’s a reason our electrophysiology colleagues exist! This article is a student-created, student-friendly guide meant for getting EKG basics down. It is perfect for those starting clinical rotations and shelf exam/Step prep. Let’s get started!
Pattern Recognition and Systematic Review
Often, EKGs can be interpreted through pattern recognition, a skill developed with practice. When patterns aren’t clear, use a systematic method to review the EKG.
Understanding Leads and Coronary Arteries
- Lead Placement:
- You don't need to memorize exact placement, but you should know the approximate areas.
- Know your cardiac anatomy!
- You can’t diagnose an MI without having an understanding of the anatomy of coronary arteries
- Understand which leads correlate with which arteries
- Leads and Corresponding Coronary Arteries
- Inferior Leads: II, III, aVF
- Right Coronary Artery (RCA) or the Left Circumflex Artery (LCx)
- Anterior Leads: V1-V4
- Left Anterior Descending Artery (LAD)
- Lateral Leads: I, aVL, V5, V6
- Left Circumflex Artery (LCx) or branches of the Left Anterior Descending Artery (LAD)
- Posterior Leads: V7-V9 (or reciprocal changes in V1-V3)
- Right Coronary Artery (RCA) or the Left Circumflex Artery (LCx)
Next: Start your systematic review
Systematic Review Steps
- Rate
- Normal/Regular: 60-100 bpm
- Tachycardia: >100 bpm
- Bradycardia: <60 bpm
- How do we figure the rate out when handed an EKG?
- 300 / number of big boxes between QRS = rate
- Rhythm
- Sinus or not sinus?
- Sinus means the rhythm originates from the SA node
- Look for the p waves!
- P wave (upright in II, III, and aVF; inverted in aVR) preceding every QRS complex and a QRS complex following every P wave
- Regular or irregular?
- Just look at the distance between QRS complexes. Is the distance the same for each? Or does it differ? That is regular vs irregular, respectively.
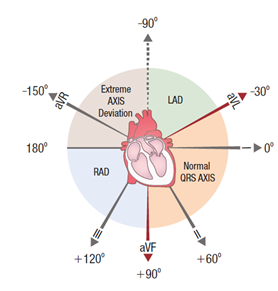
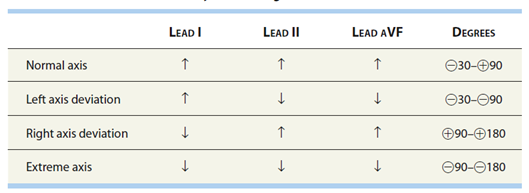
- Axis
- Normal Axis: -30° to +90°
- Left Axis Deviation (LAD): -30° to -90°
- Right Axis Deviation (RAD): +90° to +180°
- Essentially, axis abnormalities can suggest conduction abnormalities. Normally, current flows from the SA node to the left ventricle (think top right of heart to bottom left). If there is something that disrupts this flow or blocks it to some extent, the flow of current will not be exactly top right to bottom left and the axis may be deviated.
- The easy trick for determining axis deviation is:
- Hold two thumbs up in your hands
- Your left hand is lead I. Your right hand is lead AVF.
- If QRS is mostly up in those respective leads, keep the thumbs up; if the QRS is mostly down, make that hand have a thumbs down.
- If both thumbs are up, normal axis
- If one thumb is up and the other down, the axis is deviated, in the direction of the hand with the upward thumb
- Ie. QRS up in I → Left thumb up, QRS down in AVF → R thumb down, left thumb is the only one up → left axis deviation
- Intervals
- I have some bad news… this one takes some annoying memorization
- With practice you’ll be able to visualize the appropriate interval lengths, but for now try to memorize the appropriate numbers and box lengths
- PR interval: Normally 120–200 msec (3–5 small boxes).
- Prolonged = delayed AV conduction (eg, first-degree heart block).
- Short = fast AV conduction down accessory pathway (eg, WPW syndrome).
- QRS interval: Normally < 120 msec
- The QRS complex should look narrow
- Narrow means the depolarization current has traveled fast
- A wide QRS complex refers to slow ventricular depolarization
- Think about what would slow depolarization….bundle branch blocks, depolarization originating outside of the normal conduction system, etc.
- If you see a tachycardia, ask yourself is it narrow or wide?
- Narrow → originates above the ventricles (ex. A fib)
- Wide → originates at the level of the ventricular (ex. V tach)
- QT interval
- Normal: 380–440 msec
- Roughly the T wave should come before halfway to the next QRS
- Prolongation: Risk of Torsades de Pointes
Additional Findings
- ST elevations or depressions
- T Waves
- Inversion: May suggest ischemia or infarction
- Peaking: Can indicate hyperkalemia
- U Waves: Prominent in hypokalemia
Common EKG Patterns
- Myocardial Infarction (MI):
- ST Elevation MI (STEMI): ST elevation in ≥2 contiguous leads
- Non-ST Elevation MI (NSTEMI): ST depression/T wave inversion with positive cardiac biomarkers
- Atrial Fibrillation:
- Irregularly irregular rhythm with no distinct P waves
- Atrial Flutter:
- "Sawtooth" flutter waves
- Ventricular Tachycardia:
- Wide QRS complexes with a regular rhythm
- Heart Blocks:
- First-degree AV block: Prolonged PR interval (>0.20 sec).
- Second-degree AV block (Mobitz I and II): Dropped QRS complexes.
- Mobitz I: longer, longer, drop; progressive prolongation of PR until a QRS complex is dropped
- Mobitz II: no PR prolongation; sporadically dropped QRS complexes
- Third-degree AV block: Complete dissociation between P waves and QRS complexes.
Quick Tips for On-the-Spot Interpretation
When handed an EKG:
- Systematic Review: Follow the steps outlined.
- If rushed, focus on these key points:
- Rate: Tachycardia or bradycardia?
- Rhythm: Regular or irregular?
- Intervals: Any grossly abnormal intervals?
- QRS: Narrow or wide?
- ST Segments: Any elevations or depressions?
By using this structured approach, you’ll improve your EKG interpretation skills and be better prepared for clinical rotations and exams. Keep practicing, and refer back to this guide as needed.
Practice:
Oxford ECG (EKG) Examples and Quiz
EMRA Resources:
How to interpret EKGs better than you document a rash: Syncope Part 1
Related Content






