How to interpret EKGs better than you document a rash: Syncope Part 1

Flashback Friday: Lumps and Bumps: Can't-Miss Diagnoses in Syncope
Originally published February 15, 2019
In this episode Dr. Alex Kaminsky and Dr. Jeremy Berberian tackle the subtleties of syncope so you'll know how to interpret EKGs better than you document a rash.
*Spoiler alert: This throwback is also a preview! Get up to speed because we'll soon be releasing a new EMRA guide - "Emergency ECGs: Case-Based Review and Interpretations" by Jeremy Berberian, Bill Brady, and Amal Mattu.
Host
Alexander Kaminsky, MD
University of California San Francisco – Fresno
PGY4
@Alex_KamskyEM
EMRA*Cast Episodes
Guest
Jeremy Berberian, MD
Emergency medicine physician at Christiana Hospital
Associate Director of Education
Editor-in-chief : EMRA EKG Guide
Author : EMResident Monthly ECG Challenge
Hospital Affiliation: Christiana Care
EMRA Articles
Overview:
Residents are well programed to recognize cardiovascular emergencies such as STEMIs at a glance. However, during a busy shift it can be easy to overlook dysrhythmias and other electrophysiologic urgencies and emergencies. Syncope is a prime example of a chief complaint that may be uncovered with an EKG alone -- however syncopal emergencies are often subtle and nuanced. Dr. Berberian joins EMRA*Cast with Alex Kaminsky to delve deeper into the pathophysiology and electrical findings associated with diagnoses such as WPW, Brugada and ARVD in part 1 of this series.
Key Points
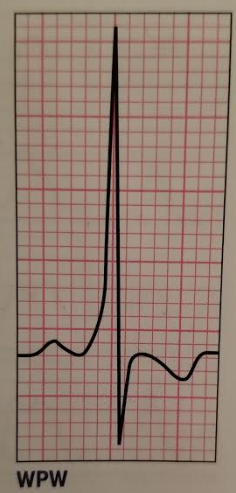
Wolff-Parkinson-White (WPW)
- Prevalence: 0.7 to 1.7 per 10,000
Overview:
Accessory Pathway Connecting the atria to the ventricle. In some instances, this can cause the accessory pathway to travel FASTER than through the AV node.
- Orthodromic (Narrow): Travels down the AV node (can bypass)
- Antidromic (Wide): Bypasses AV node and UP the his-purkinje system.
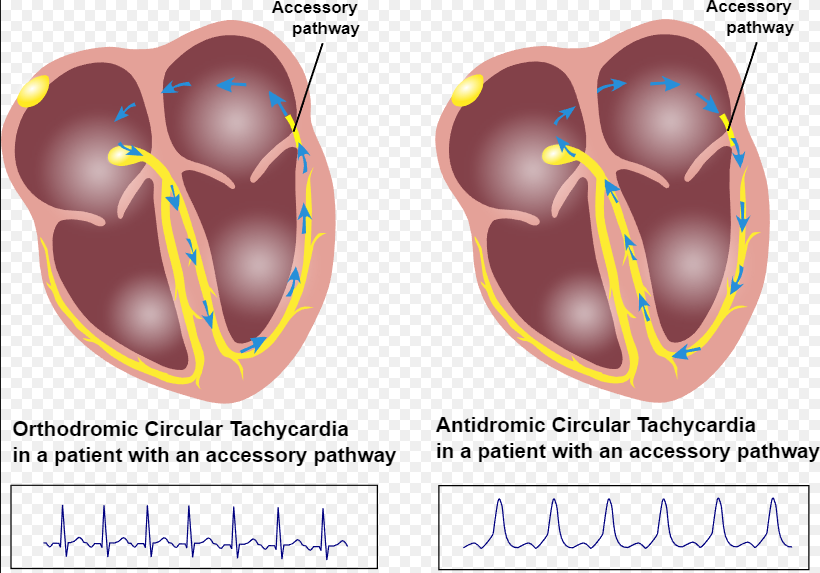
Courtesy of CardioNetworks: Free use image
Key Features:
|
Image Courtesy of EMRA EKG Guide |
Most common presentation is SVT. But also can present as atrial fibrillation. |
Treatment:
Orthodromic (Narrow): Treat like SVT
Key Point: Procainamide is the most safe chemical cardioversion in WPW as it does not directly affect the AV node. Use of AV-nodal blockers in WPW (including Amiodarone) increases the risk of VT/VF.
***Blocking the AV node in a WPW patient in Atrial Fibrillation can precipitate bad ventricular rhythms. If you see A-fib GREATER than 220 minus age -- consider WPW.***
Antidromic (Wide): Treat Like V-Tach
Braguda Syndrome:
- Prevalence: 5 in 10,000. Traditionally taught more common in Southeast Asian populations.
Overview:
- Sodium Channelopathy which can lead to unstable dysrhythmias and ultimately cardiac death.
Key Features:
- Diagnosis is made both by EKG and clinical criteria
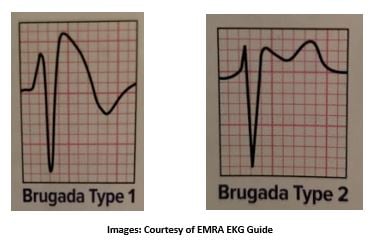
Type 1:
- “Coved” ST-Elevation >2mm with a negatively deflected T in right precordial leads (V1-V3)
- Potentially diagnostic as isolated EKG finding.
Type 2:
- ST elevation in right precordial leads (V1-V3) with a “saddleback.” Within the STE.
- Not completely diagnostic but concerning fr workup.
Clinical Criteria (EKG Findings PLUS one or more):
- SYNCOPE
- Nocturnal Agonal Respirations
- Brugada gets WORSE with parasympathetic stimuli.
- Family member with known Type 1
- Observed/Documented VT/VF
- Sudden cardiac death in family member <45 (Take that history!)
Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy (ARVD)
- Prevalence: Unknown, likely more than we thought. Mean age is 31. Also we don’t have great clinical criteria to full encompass this -- yet. Multiple genes linked to disease process. Variable inheritance patterns.
Overview:
- Fibro-Fatty infiltration of the myocardium that replaces good “conductive” tissue with fibrinous infiltrates. Think: “Kinda like cirrhosis of the heart.”
- Causes paroxysmal ventricular rhythms. Can present as CHF.
Key Features:
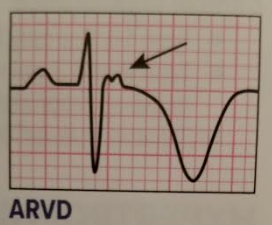
Image Courtesy of EMRA EKG Guide
- Epsilon wave -- AKA “The Ditzle or Nubbin” (only in 30% of patients)
- T-wave inversions in right precordial leads (V1-V3) -- (85% of patients)
- Long S-wave repolarization delay >55ms (in 95% of patients)
- Slightly prolonged QRS >110ms (Right precordial leads)
- VT looks more like a Left-bundle morphology -- Appreciate that AFTER the patient is out of VT.
References / Resources
- EMRA EKG Guide
- Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients Presenting to the Emergency Department with Syncope: Huff J.S., Decker W.W., Quinn J.V., Perron A.D., Napoli A.M., Peeters S., Jagoda A.S.( 2007) Annals of Emergency Medicine, 49 (4) , pp. 431-444.
- Epidemiological profile of Wolff-Parkinson-White syndrome in a general population younger than 50 years of age in an era of radiofrequency catheter ablation. Lu C.-W., Wu M.-H., Chen H.-C., Kao F.-Y., Huang S.-K. (2014) International Journal of Cardiology, 174 (3) , pp. 530-534.
- Reference, G. (2019). Brugada syndrome. [online] Genetics Home Reference. Available at: https://ghr.nlm.nih.gov/condition/brugada-syndrome#statistics [Accessed 14 Feb. 2019].
- McNally E, MacLeod H, Dellefave-Castillo L. Arrhythmogenic Right Ventricular Cardiomyopathy. 2005 Apr 18 [Updated 2017 May 25]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1131/
Related Content

Jan 17, 2024
Optimism vs. Realism — Let’s Call it a Tie
As the voice of emergency medicine physicians-in-training and the future of our specialty, EMRA continues to believe that the future of EM is bright while remaining committed to facing reality and addressing our headwinds. I invite you all to join us in this Stockdale Paradox-esque approach.