The prompt identification of a potential environmental toxin allows for early treatment and management. Specific identification as well as recognition of pertinent signs and symptoms are important skills for everyone who spends time outdoors.
Many plants found in various regions can result in toxic effects when encountered by humans. Whether through direct cutaneous contact, ingestion, or other exposure, many plants can exhibit a local or systemic reaction. Try to identify the following flora from the photo and clinical history.
Patient #1
You are working in an ED in Texas when EMS brings you a 20-year-old male who “isn’t acting right.” He is flushed, tachycardic, febrile, and has completely dry skin. He states that he and his friends were eating a plant they found in the woods, “trying to get high.” He shows you a picture of the plant.

Patient #2
You are out hiking in the woods in rural South Carolina when your friend goes off the trail through a patch of low brush. Soon after, he begins to experience significant redness, itching, and small blisters over his legs. You look closer at the area where he walked and see this…

Patient #3
A patient presents to the ED in Ohio complaining of chest pain and “passing out.” He states that he is a forager and has been eating leaves from a plant he thought was safe. He shows you what he’s been eating.

Patient #4
A hiker calls 911 after finding his 3-year-old son eating mushrooms from a small patch during a family camping trip in central California. He was able to take a picture of the mushroom and showed the first responders.

Patient #5
A woman is brought to the ED with hypotension (BP 60s/40s), bradycardia (40 bpm), and vomiting. Electrocardiography reveals ST depressions in inferior leads. The patient was slow to respond to verbal stimuli, but exam was otherwise non-focal. While preparations are made to take the patient for cardiac intervention, further history reveals that symptoms began shortly after having consumed honey that was brought to her from a Turkish friend.

Patient #6
A 17-year-old male is brought to the ED after ingesting multiple beans as pictured. He blended them with juice and drank the mixture in an attempt to commit suicide. He presents shortly after ingestion, with nonspecific symptoms including weakness, nausea, vomiting, and abdominal pain.

Patient #7
A toddler presents to an urban ED with swelling of the lips and tongue with irritated, painful mucosa. The posterior oropharynx appears benign and there is no stridor or respiratory distress. The patient’s mother brings in several large leaves from one of their houseplants. She reports the child was chewing on them shortly before symptoms began.

Patient #8
A foraging hobbyist is brought in by ambulance having a seizure. He found a “parsnip variety” near a pond in New York City’s Central Park. His companion brings in a picture of the plant. An experienced forager from the Midwest, he followed his usual strategy of tasting a small part of the plant before planning to cook with it the next day. He has never had a problem when eating “water parsnip” before.

Answers and Summary
Early identification of a possible plant-based toxin or exposure can greatly assist in the management and stabilization of an affected individual. In general, eliminating potential additional exposure and commencing supportive care are the first-line treatment of many environmental toxins.
Become familiar with the specific toxic plants that may be found in your region, and be prepared when exploring outdoors or providing care. Know the contact information for your local poison control center and discuss exposures with them for up-to-date treatment and management options.
Patient #1: Jimsonweed (Datura stromonium)

The patient likely ingested Datura stromonium or Jimsonweed. The seeds, stems, leaves, and roots can be ingested or smoked in an attempt to obtain hallucinogenic effects. However, this can result in an anticholinergic toxidrome in an exposed individual due to the presence of atropine, L-hyoscyamine, and L-scopolamine, inhibiting the peripheral and central muscarinic acetylcholine receptors.1 Symptoms include agitation, delirium, fever, tachycardia, dry skin and mucous membranes, skin flushing, diminished bowel sounds, and urinary retention.2,3 The treatment of an acute toxic exposure is largely supportive, and driven by symptoms. Specific anticholinergic antidotes for significant intoxication including physostigmine can be administered usually after discussion with a specialist.2,4
Patient #2: Poison oak (Toxicodendron diversilobum)

The likely culprit is poison oak (Toxicodendron diversilobum). Other plants that commonly cause allergic dermatitis include poison ivy (T. radicans) and poison sumac (T. vernix).
Poison ivy can be identified as a short vine or shrub with groups of 3 long, oval leaves with an apex point. The “common” or Eastern version can be found in the Eastern United States and Southern Canada, while the Western variety is found in Western states except California.
Poison oak can be found along the Pacific Coast and Southeastern United States, and it is identified by stems with groups of 3-5 oval leaves 3-7 cm long with wavy to deeply lobed margins and a rounded tip.
Poison sumac is found mostly in wet, marshy regions of the Southeastern United States and can be identified by having groups of 7-13 leaves arranged as pairs along a central stalk, with a single leaflet at the end.5,6
Exposure to all varieties can cause a localized contact dermatitis because of a Type IV hypersensitivity reaction to the compound oleoresin urushiol found in the leaves, stems, berries, and roots.7,8 Symptoms usually present within 24-48 hours from exposure in a previously sensitized individual and can include intense pruritus and erythema, followed by vesicles and bulla.5 Treatment includes symptom control with topical steroids, cool compresses, and antihistamines for localized cases, and oral steroids for more serious reactions. The lesions will likely heal on their own in 7-10 days.6,8

Poison Ivy (T. radicans)

Poison Sumac (T. vernix)
Patient #3: Foxglove (Digitalis purpurea)

These bright flowers come from the foxglove (Digitalis purpurea) plant. This and many other wild plants contain potent chemicals that affect the heart, called cardiac glycosides (including digoxin).9 Poisonings after ingestions of this plant display similar characteristics as digitalis toxicity, including nausea, vomiting, visual disturbances, abdominal pain, hyperkalemia, A/V conduction blocks, bradycardia, and ventricular tachydysrhythmias including bidirectional ventricular tachycardia.10,11 Supportive care is the mainstay of treatment, but obtaining a serum digoxin level may help make a definitive diagnosis. However, the quantitative value does not correlate with the degree of toxicity from exposure to a non-pharmaceutical cardiac glycoside and should not be used to guide antidote dosage.11
Patient #4: Death Cap (Amanita phalloides)

This mushroom is the deadly Amanita phalloides or “death cap.” All parts of the mushroom contain toxins, with amatoxin as the main agent causing effects in humans.12,13,14 The liver is the primary organ affected, but the kidneys and other organs are also impacted. Amatoxins inhibit RNA synthesis and prevent protein synthesis, inhibiting normal liver regenerative capacity and leading to hepatic failure.13,14 Symptoms usually appear after a latent period and include abdominal pain, nausea, and vomiting followed by jaundice, seizures, coma, and ultimately death.13 The main treatment options include supportive care and potentially liver transplant if there is progression to complete liver failure.12
Patient #5: Rhododendron

The patient is suffering from poisoning from grayanotoxin found in the honey, which was produced near rhododendron in bloom. Concentration of grayanotoxin in the honey leads to “mad honey disease,” which is marked by hypotension, bradycardia, nausea, vomiting, and somnolence due to the effect on sodium channels and the M2 receptor. Treatment includes supportive care and atropine.15
Patient #6: Castor beans (Ricinus communis)

The ingestion of castor seeds may cause mild symptoms but commonly proves to be fatal. The content of ricin in castor beans varies widely, and the bioavailability depends heavily on mechanical separation from the beans, as in chewing or grinding. Castor beans from Ricinus communis are among the most toxic readily available plants. Ricin, a protein toxin found in the seeds, is inactivated with cooking, as in the preparation of castor oil. Its toxicity stems from inhibition of protein synthesis. Ingestion of ricin can lead to nausea, vomiting, abdominal pain, GI hemorrhage, and possibly death. Other routes of exposure such as inhalation and parenteral injection are more deadly and of concern for acts of terrorism. Specific testing for ricin is potentially difficult, but another specific small molecule, ricinine, is readily detectable by gas chromatography-mass spectrometry.16
Patient #7: Elephant’s ear

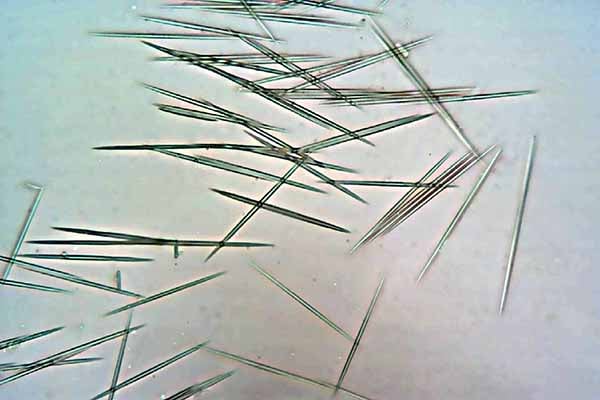
Raphides are an insoluble crystalline form of oxalate that is present in a variety of common household and agricultural plants including the leaves of elephant’s ear, pineapple, kiwi fruit, and others. Oral exposure leads to physical irritation to tissues including pain and edema that, in rare instances, can lead to airway compromise.17 Treatment is symptomatic and supportive. Other types of plants have similar raphides, and common placement of these in households as decorations can lead to accidental exposure.
Patient #8: Water hemlock (Cicuta maculata)

Water hemlock (Cicuta maculata) contains cicutoxin in large quantities in its root bulb. It is considered one of the most toxic plants in North America and is prevalent in waterways in North America.18 There are many edible plants that have a similar appearance, including water parsnip.19
Image Credits
1. WikimediaImages. “Datura Stromonium.” (https://pixabay.com/en/datura-stramonium-jimson-weed-844548). CC0 1.0
2. Folini, Franco. “Pacific poison oak.” (https://www.flickr.com/photos/livenature/5798481272) CC BY-SA 2.0
3. JamesDeMers “Poison Ivy.” (https://pixabay.com/en/poison-ivy-toxicodendron-radicans-195123/). CC0 1.0
4. Mayer, Joshua. “Poison Sumac (Toxicodendron vernix)” (https://www.flickr.com/photos/wackybadger/24924876934). CC BY-SA 2.0
5. Music4Life “Common Foxglove.” (https://pixabay.com/en/common-foxglove-wild-plant-thimble-2400621/). CC0 1.0
6. Archnzo. “Amanita phalloides.” (https://commons.wikimedia.org/wiki/File:Amanita_phalloides_1.JPG) CC BY-SA 3.0
7. Opioła, Jerzy. “Rhododendron catawbiense a2” (https://commons.wikimedia.org/wiki/File:Rhododendron_catawbiense_a2.jpg). CC BY 3.0
8. Unknown. “Castor Beans.” (https://commons.wikimedia.org/wiki/File:Castor_beans.jpg). Public Domain
9. Joliff, Heath “Elephant Ear.”
10. Agong1. “Raphides in Epipremnum Devil's ivy” (https://en.wikipedia.org/wiki/Raphide#/media/File:Raphides_from_variegated_ivy.jpg). CC0 1.0
11. Fritzflohrreynolds. “Cicuta maculata - Water Hemlock.” (https://commons.wikimedia.org/wiki/File:Cicuta_maculata_-_Water_Hemlock.jpg). CC BY-SA 3.0
References
1. Trancă SD, Szabo R, Cocis M. Acute Poisoning Due to Ingestion of Datura Stramonium – a Case Report. Rom J Anaesth Intensive Care. 2017;24(1):65-68.
2. Salen P, Shih R, Sierzenski P, Reed J. Effect of Physostigmine and Gastric Lavage in a Datura Stramonium-Induced Anticholinergic Poisoning Epidemic. Am J Emerg Med. 2003;21(4):316-317.
3. Soulaidopoulos S, Sinakos E, Dimopoulou D, Vettas C, Cholongitas E, Garyfallos A. Anticholinergic Syndrome Induced by Toxic Plants. World J Emerg Med. 2017;8(4):297-301.
4. Watkins JW, Schwarz ES, Arroyo-Plasencia AM, Mullins ME, Toxicology Investigators Consortium Investigators. The Use of Physostigmine by Toxicologists in Anticholinergic Toxicity. J Med Toxicol. 2014;11(2):179-184.
5. Gladman AC. Toxicodendron Dermatitis: Poison Ivy, Oak, and Sumac. Wilderness Environ Med. 2006;17(2):120-128.
6. Freeman E. Plant-Induced Dermatitis. In: Auerbach PS, ed. Auerbach's Wilderness Medicine. New York City, NY:Elsevier;2017:1413–1433.
7. Lee NP, Arriola ER. Poison Ivy, Oak, and Sumac Dermatitis. West J Med. 1999;171(5-6):354-355.
8. Vaught CK, Mold JW. Poison ivy: How effective are available treatments? J Fam Pract. 2016;65(11):801-809.
9. Lin CC, Yang CC, Phua DH, Deng JF, Lu LH . An Outbreak of Foxglove Leaf Poisoning. J Chin Med Assoc. 2010;73(2):97-100.
10. Diaz JH. Poisoning by Herbs and Plants: Rapid Toxidromic Classification and Diagnosis. Wilderness Environ Med. 2016;27(1):136-152.
11. Janssen RM, Berg M, Ovakim DH. Two Cases of Cardiac Glycoside Poisoning from Accidental Foxglove Ingestion. CMAJ. 2016;188(10):747-750.
12. Diaz JH. Amatoxin-Containing Mushroom Poisonings: Species, Toxidromes, Treatments, and Outcomes. Wilderness Environ Med. 2018;29(1):111-118.
13. Garcia J, Costa VM, Carvalho A, Baptista P, de Pinho PG, de Lourdes BM, Carvalho F. Amanita Phalloides Poisoning: Mechanisms of Toxicity and Treatment. Food Chem Toxicol. 2015;86:41-55.
14. Vetter J. Toxins of Amanita Phalloides. Toxicon. 1998;36(1):13-24.
15. Broscaru L, Dobre C, Rosick F, Halilovic A, Gulba D. Mad Honey Disease. Eur J Case Rep Internal Med. 2017;5(1).
16. Lopez Nunez OF, Pizon AF, Tamama K. Ricin Poisoning after Oral Ingestion of Castor Beans: A Case Report and Review of the Literature and Laboratory Testing. J Emerg Med. 2017;53(5):e67-e71.
17. Cumpston KL, Vogel SN, Leikin JB, Erickson TB. Acute airway compromise after brief exposure to a Dieffenbachia plant. J Emerg Med. 2003;25(4):391-397.
18. Cetaruk EW. Water Hemlock. In: Brent J, ed. Critical Care Toxicology: Diagnosis and Management of the Critically Poisoned Patient. Berlin, Germany: Springer; 2017:2225–2236.
19. Landers D, Seppi K, Blauer W. Seizures and death on a white river float trip-Report of water hemlock poisoning. West J Med. 1985;142(5):637-640.



