A missed diagnosis of Wernicke encephalopathy (WE) can lead to Korsakoff syndrome, which carries a 20% mortality rate. Because this life-threatening condition can be easily misdiagnosed, it's important to recognize the signs.
Case
A 34-year-old female is brought to the ED with a chief complaint of "altered mental status." A neighbor called EMS after she found the patient unable to walk and noted she was "acting strangely." Chart review reveals that the patient underwent a sleeve gastrectomy 7 months ago complicated by 2 months of post-operative hyperemesis as well as a remote history of polysubstance use disorder. She has missed most of her follow-up appointments with bariatric surgery. The patient is alert to self, but not to place, time. She answers questions in complete sentences; although, her answers are tangential and nonsensical. Physical exam reveals horizontal nystagmus, bilateral lower extremity weakness, and significant dysmetria.
 Wernicke encephalopathy (WE) is an acute neurological complication of thiamine deficiency characterized by altered mental status, oculomotor dysfunction, and ataxia. Korsakoff syndrome is a late, chronic manifestation of WE that typically presents as anterograde and retrograde amnesia with intact long-term memory.
Wernicke encephalopathy (WE) is an acute neurological complication of thiamine deficiency characterized by altered mental status, oculomotor dysfunction, and ataxia. Korsakoff syndrome is a late, chronic manifestation of WE that typically presents as anterograde and retrograde amnesia with intact long-term memory.
Autopsy studies estimate a prevalence of approximately 1.3% in the general population and as high as 9% in chronic alcohol users. It is significantly underdiagnosed. Only 70% of patients with alcohol use disorder and post-mortem evidence of WE were diagnosed antemortem. 90% of WE cases in industrialized nations are associated with alcohol use disorder. After alcohol use disorder, the most common causes of WE are cancer (1.8%), gastrointestinal surgery (1.7%), hyperemesis gravidarum (1.2%), and starvation/fasting (1%).1
The exact incidence of Korsakoff syndrome is unclear. Untreated WE advances to Korsakoff syndrome in 56-85% of patients and leads to death in approximately 20%.2
Pathophysiology
Thiamine is a cofactor for pyruvate dehydrogenase and alpha-ketoglutarate dehydrogenase. It is needed for pyruvate to enter the citric acid cycle to allow for aerobic metabolism of glucose to adenosine triphosphate (ATP). Lack of ATP production in areas of the brain susceptible to thiamine depletion leads to neuronal death. WE lesions are characterized by petechial hemorrhages and are most often found in a symmetrical distribution around the third ventricle, cerebral aqueduct, and fourth ventricle.
Thiamine deficiency is most often multifactorial. In patients with alcohol use disorder, the etiology is threefold: inadequate nutritional intake, reduced hepatic storage, and inhibition of intestinal thiamine transporters by ethanol. Genetic variations in the affinity between thiamine and thiamine transporters may contribute to variable individual susceptibility to WE.3-6
Korsakoff syndrome is much less frequent in cases of WE that are not associated with alcohol use, suggesting that ethanol may have a direct neurotoxic role in its development.2,7
Clinical Features
The classic triad of WE is encephalopathy, oculomotor dysfunction, and gait ataxia. However, only 8.2% of patients present with all three symptoms. 53% of patients present with altered mental status, 25% with cerebellar signs, 24% with ocular signs, and 23% with amnesia. The encephalopathy is characterized by disorientation and inattention. Nystagmus and ophthalmoplegia are the most common ocular findings.1
Other symptoms seen include vestibular dysfunction, peripheral neuropathy, hypothermia, and tachycardia. Given the nonspecific presentation, it is essential to maintain a high index of suspicion of WE in any patient with a potential source of malnutrition.
The diagnosis of WE is clinical. Normal serum thiamine levels do not rule out WE as they may not accurately represent brain thiamine levels. Imaging is not necessary to diagnosis WE but may be useful to rule out other etiologies. Mammillary body atrophy is the most specific radiological finding in patients with WE, though it is not diagnostic.8,9
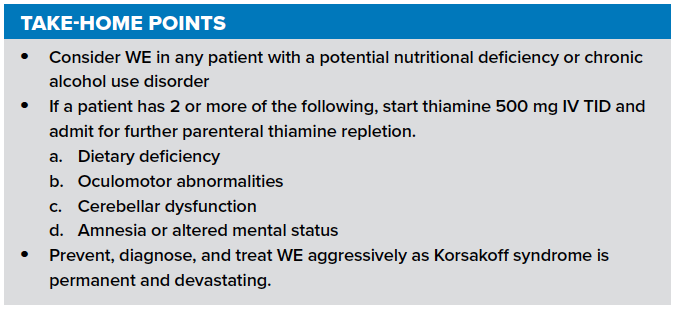
Presence of 2 of the 4 Caine criteria can assist in making the diagnosis and have a specificity of 87%.10
Caine Criteria
- Dietary deficiency
- Oculomotor abnormalities
- Cerebellar dysfunction
- Altered mental status or mild memory impairment
Korsakoff syndrome typically presents as anterograde and retrograde amnesia with intact long-term memory. Some patients also display confabulation: the unconscious production of fabricated memories. Other areas of higher cognitive functioning are generally preserved; although, some patients may develop global dementia. The onset of Korsakoff syndrome usually presents as a progression of clinical WE syndrome. However, some patients may have subclinical WE, and initially present with Korsakoff symptoms only. Patients with Korsakoff syndrome seldom recover memory function.11,12
Management
Patients with signs and symptoms concerning for WE require high dose parenteral thiamine. The exact dose and duration are debated. Standard practice is to start thiamine 500 mg IV infused over 30 minutes, given 3 times daily. Patients should be admitted, as they will need at least 5 days of IV thiamine. These patients frequently have mixed vitamin deficiency. Thus, they should also be started on a B-complex multivitamin as well.
Malnourished patients should receive thiamine before, or in tandem with, glucose loading as the glucose load may induce thiamine deficiency. However, the evidence for this is limited, and glucose administration should not be delayed if needed.13
In WE, ocular palsies should resolve over hours to days, and confusion should resolve within days to weeks. Almost all patients exhibit some residual deficits.14
Almost no patients recover memory function after the onset of Korsakoff syndrome. Small case series have evaluated the use of memantine for patients with Korsakoff with some success. Although there is limited evidence to support it, the devastating effects of Korsakoff syndrome may justify its use in some cases. Patients with Korsakoff syndrome often require long-term care.15
Prevention
Current practice guidelines recommend that chronic alcohol users should receive parenteral thiamine supplementation to prevent the onset of WE. There is insufficient evidence to determine the optimal dose or route of prophylactic thiamine or to establish its efficacy. The risks and cost of thiamine are extremely low and are significantly outweighed by the potential benefits.1,16,17
Case Resolution
When you return to the patient’s room after several minutes, she states that she met you last week. A non-contrast head CT shows no intracranial pathology. The patient is started on high dose thiamine and admitted to neurology for further workup and management. Her motor and cerebellar symptoms improve over the next month, however, the amnesia persists and she is eventually discharged to a long-term care facility.
References
1. Galvin R, Brathen G, Ivashynka A, Hillbom M, Transescu R, Leone M. EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. Eur J Neurol. 2010;17(12):1408-1418.
2. Thomson A, Marshall EJ. The natural history and pathophysiology of Wernicke’s encephalopathy and Korsakoff’s psychosis. Alcohol Alcohol. 2005;41(2):151-158.
3. Thomson AD, Pratt OE, Jeyasingham M, Shaw GK. Alcohol and brain damage. Hum Toxicol. 1988;7(5):455-63.
4. Guerrini I, Thomson AD, Cook CC, et al. Direct genomic PCR sequencing of the high affinity thiamine transporter (SLC19A2) gene identifies three genetic variants in Wernicke Korsakoff syndrome (WKS). Am J Med Genet B Neuropsychiatr Genet. 2005;137B(1):17-9.
5. Thomson AD, Ryle PR, Shaw GK. Ethanol, Thiamine and Brain Damage. Alcohol Alcohol. 1983;18(1):27-43.
6. Hoyumpa AM Jr. Mechanism of Thiamine deficiency in chronic alcoholism. Am J Clin Nutr. 1980;33(12):2750-61.
7. Freund G. Chronic central nervous system toxicity of alcohol. Annu Rev Pharmacol. 1973;13(1):217-27.
8. Davies SB, Joshua FF, Zagami AS. Wernicke's encephalopathy in a non-alcoholic patient with a normal blood thiamine level. Med J Aust. 2011;194(9):484-4.
9. Charness ME. Intracranial voyeurism: revealing the mammillary bodies in alcoholism. Alcohol Clin Exp Res. 1999;23(12):1914-4.
10. Caine D, Halliday GM, Kril JJ, Harper CG. Operational criteria for the classification of chronic alcoholics: identification of Wernicke's encephalopathy. J Neurol Neurosurg Psychiatry. 1997;62(1):51-60.
11. Torvik A, Lindboe CF, Rogde S. Brain lesions in alcoholics: a neuropathological study with clinical correlations. J Neurol Sci. 1982;56(2):233-48.
12. Victor, M, Adams, RA, Collins, GH. The Wernicke-Korsakoff syndrome and related disorders due to alcoholism and malnutrition. Mayo Clin Proc. Philadelphia 1989.
13. Schabelman E, Kuo D. Glucose before thiamine for Wernicke encephalopathy: a literature review. J Emerg Med. 2012;42(4):488-94.
14. Foster JB. The Wernicke-Korsakoff Syndrome and Related Neurologic Disorders Due to Alcoholism and Malnutrition. 2nd Edition. J Neurol Neurosurg Psychiatry. 1989;52(10):217-1218.
15. Rustembegović A, Kundurović Z, Sapcanin A, Sofic E. A placebo-controlled study of memantine (Ebixa) in dementia of Wernicke-Korsakoff syndrome. Med Arh. 2003;57(3):149-50.
16. Day E, Bentham PW, Callaghan R, Kuruvilla T, George S. Thiamine for prevention and treatment of Wernicke-Korsakoff Syndrome in people who abuse alcohol. Cochrane database Syst Rev. 2013;(7):CD004033.
17. Wrenn KD, Murphy F, Slovis CM. A toxicity study of parenteral thiamine hydrochloride. Ann Emerg Med. 1989;18(8):867-70.



