In the ED, acute arrhythmias — including paroxysmal supraventricular tachycardias (pSVT) — gather much attention.
Upon recognition of the arrhythmia, there is often a storm of actions including EKGs, intravenous access, and defibrillator pad application. A patient who is already experiencing symptoms of palpitations, chest pain, or dyspnea will frequently be disturbed by the sensations and experience a sympathetic adrenergic response.
Pediatric patients in this situation will often and understandably have difficulty controlling their emotions. While this is a common occurrence with 1.26 million cases estimated episodes in 2018 alone,1 treatment of pSVT itself comes with a sense of urgency, a need to act and reach for reliable medications such as adenosine to “break” them from their abnormal rhythm.
It is worth considering that adenosine administration can compound the problem by causing distinctly uncomfortable symptoms associated with the sino-atrial pause. Calcium channel blockers (CCBs), which were a previously commonly used pharmacologic tool for pSVT, can offer a reliable and smoother transition from a tachyarrhythmia to a normal sinus rhythm in a more comfortable way for the patient.2
In this case report, we depict how verapamil was used in an extremely anxious child with autism during a pSVT episode to restore him to a normal sinus rhythm with no complications.
Case Description
The patient in question, transferred from a local urgent care facility, was a 10-year-old male with autism spectrum disorder and new onset supraventricular tachycardia (SVT). Per the family, the patient awoke at midnight complaining of chest pain and palpitations. His mother, a former nurse, noted that his heart rate was beating fast and took the patient to an urgent care center. At the urgent care center, vagal maneuvers of blowing into a syringe and ice water to the face (so-called “dive reflex”) were attempted but unsuccessful. The patient was extremely anxious despite intranasal midazolam and resistant to placement of an intravenous catheter. At 100kg, he was strong enough to make restraint impossible to safely perform by the staff at the urgent care facility. The patient was transferred to the nearest pediatric referral hospital for management of his SVT and for cardiology evaluation.
On arrival, the patient continued to complain of chest pain, was extremely anxious, and threatened violence in response to attempts at IV access. The mother noted the patient had a history of escalation. Verbal redirection, negotiation, and maternal efforts at de-escalation all failed. Intramuscular ketamine was used to transiently sedate the patient to allow us to get IV access. With the patient sedated, we were able to attach the cardiac monitor/defibrillator and get a reliable EKG showing a narrow complex tachycardia consistent with pSVT with a rate of 208 bpm (Figure 1). Given the significant anxiety of the patient and his poor coping mechanisms, an effort was made to avoid the unpleasant side effects that accompany adenosine. The decision was made to use a CCB.
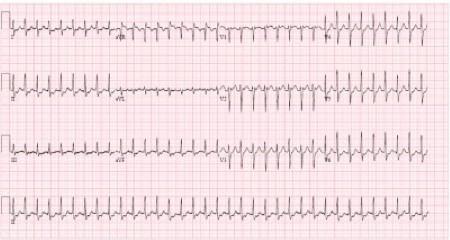
Figure 1: Paroxysmal SVT. Note the tachycardia (>200 bpm) with a regular rhythm and the lack of evidence of a delta wave.
After attaching the cardiac monitor, preparing the room, and outlining the plan with the care team and family, we gave the patient 5 mg of intravenous verapamil over a 2-minute slow push. In the next 5 minutes, the patient’s heart rate steadily trended downward from greater than 200 to 180 before abruptly converting to 110 beats per minute. Repeat EKG at that time showed a pediatric normal sinus rhythm (Figure 2). The patient expressed no discomfort or startle response to the heart rate change. The patient was observed in the ED for 1 hour with no resumption of his SVT. He was then transferred to the pediatric intensive care unit for close cardiac monitoring. No further episodes were reported. A follow-up echocardiogram showed no structural abnormalities. The patient was discharged to cardiac follow-up on no new medications.
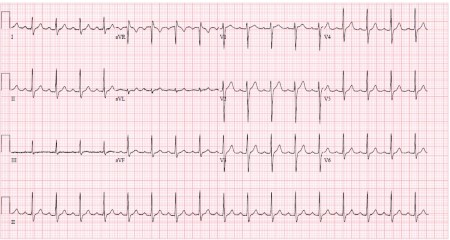
Figure 2: Normal pediatric sinus rhythm
Discussion
Paroxysmal supraventricular tachycardia (pSVT) is an umbrella term that can refer to one of several pathologies, such as atrioventricular node re-entrant tachycardia and less commonly atrioventricular reciprocating tachycardia, as well as several other less common atrial tachycardias. Together, these pathologies represent a circling electrical depolarization occurring within the atria, above (or within) the atrioventricular node. The methods of treating pSVT generally modulate the AV node with vagal maneuvers, pharmacokinetics, or cardioversion to terminate the re-entrant depolarization.3
The management of a patient with pSVT is primarily determined by their blood pressure; as with most tachyarrhythmias, hypotensive patients receive cardioversion (usually 0.5J/kg). Next, it is important to examine the EKG for QRS width and regularity. A narrow, regular QRS complex without preceding P-waves indicates that AV nodal blocking may be safe. However, irregular, wide complexes should prompt concern for the presence of an accessory pathway, which can result in ventricular fibrillation.
If there are no barriers, the first attempt to break the pSVT is often a vagal maneuver such as bearing down, dive reflex, or leg lifts. These maneuvers work by stimulating the vagus nerve, which directly inhibits the AV node, and are frequently sufficient to terminate the re-entrant cycle. Bearing down with and without leg lifting afterward is successful 43% and 17% of the time, respectively. If vagal maneuvers are not successful, then a pharmacologic intervention is usually required.4
Adenosine vs. Calcium Channel Blockers
Adenosine acts as a strong atrioventricular nodal blocking agent with a short half-life (less than 1 minute). It must be administered aggressively and meticulously to ensure a brief but full block of the AV node; a slow push or inexperienced administration can result in a failure.
Dosage of adenosine is well understood — 0.1mg/kg for the first dose (maximum of 6mg) followed by 0.2mg/kg (maximum of 12mg) for the second and third doses.2 Unfortunately, adenosine has short-lived but very unpleasant adverse reactions of dyspnea, chest pain, and a sense of impending doom.5
Non-dihydropyridine CCBs like verapamil and diltiazem are the classic CCBs used for pSVT. CCBs act by inhibiting the calcium movement across the cardiac cell membrane, delaying cascade depolarization. This effect is most prominent in the electrical conduction system (the SA and AV nodes) and results in perturbing the re-entrant cycle, allowing a normal sinus rhythm to resume. Diltiazem is dosed at 0.25mg/kg IV over 2 minutes with a re-bolus at 15 minutes later of 0.35mg/kg as needed.6 Verapamil is contraindicated in infants as there have been rare reports of asystole and hypotension, but it is usually well-tolerated with an IV dose of 0.1mg/kg (maximum 5mg) and subsequent doses of 0.2 mg/kg (maximum 10mg) as needed.7,8
When compared to adenosine, CCBs are inexpensive, require less coordination for administration of the medication, and are not accompanied by the same patient discomfort. CCB side effects worth considering are hypotension and dizziness; much more rarely AV block and pulmonary edema can occur. Prophylactic doses of calcium infusions can reduce the effect of verapamil-induced hypotension and improve efficacy of the verapamil bolus.9 Either adenosine or verapamil can be used safely in pregnant or breastfeeding mothers.10
Take-Home Point
When a pediatric patient presents to the emergency department with pSVT and vagal maneuvers have failed, choice of AV nodal blocking agent is important. This case shows that CCBs offer several advantages over adenosine, which should prompt a more careful consideration of which agent to use in pediatric patients. Adenosine is the first-line agent, but it is worth pausing to consider the benefits of alternative agents.
References
- Rehorn M, Sacks NC, Emden MR, et al. Prevalence and incidence of patients with paroxysmal supraventricular tachycardia in the United States. J Cardiovasc Electrophysiol. 2021;32(8):2199-2206.
- Ahmad F, Sneineh MA, Patel RS, et al. In The Line of Treatment: A Systematic Review of Paroxysmal Supraventricular Tachycardia. Cureus. 2021;13(6).
- Colucci RA, Silver MJ, Shubrook J. Common Types of Supraventricular Tachycardia: Diagnosis and Management. Am Fam Physician. 2010;82(8):942-952.
- Appelboam A, Reuben A, Mann C, et al. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial. The Lancet. 2015;386(10005):1747-1753.
- Alabed S, Sabouni A, Providencia R, Atallah E, Qintar M, Chico TJ. Adenosine versus intravenous calcium channel antagonists for supraventricular tachycardia. Cochrane Database Syst Rev. 2017;(10).
- Sternbach GL, Schroeder JS, Eliastam M, Beier-Scott L. Intravenous diltiazem for the treatment of supraventricular tachycardia. Clin Cardiol. 1986;9(4):145-149.
- Schamroth L, Krikler DM, Garrett C. Immediate Effects of Intravenous Verapamil in Cardiac Arrhythmias. Br Med J. 1972;1(5801):660-662.
- Verapamil: Generic, Hypertension, Uses, Side Effects, Dosages, Interactions, Warnings. RxList. Accessed April 29, 2022.
- Lim SH, Anantharaman V, Teo WS, Chan YH. Slow infusion of calcium channel blockers compared with intravenous adenosine in the emergency treatment of supraventricular tachycardia. Resuscitation. 2009;80(5):523-528.
- Tan HL, Lie KI. Treatment of tachyarrhythmias during pregnancy and lactation. Eur Heart J. 2001;22(6):458-464.



