Prevention, Clinical Manifestation, Diagnosis, and Checklist for Management
While rotating in the emergency department and in the intensive care unit, residents are responsible for inserting and removing an assortment of central venous catheters (CVC) for various reasons, whether it is for emergent dialysis, rapid infusion of large resuscitation volumes, or for continued support of medical therapy.
Although the Accreditation Council for Graduate Medical Education (ACGME) requires the application of at least 20 CVCs by the time of residency completion, this procedure is relatively common, allowing for residents to place a significant more during their training, thereby allowing them to become increasingly proficient. While the techniques involved can be monotonous, it is critical for the operator to remain cognizant of the complications that can occur with catheter insertion and removal, including one of the most feared, which is a venous air embolism (VAE).
What is a venous air embolism (VAE)?
VAE occurs when air or gas is introduced to the venous system. The volume and the infusion rate both determine severity of symptoms and presentation.4 While 300-500 mL of gas introduced at a rate of 100 mL/sec can be acutely fatal for humans, volumes as low as 50 mL have been reported to be fatal.
Large air bubbles cause obstruction of pulmonary outflow tract and pulmonary vessels; this obstruction causes decreased blood return from right ventricle, increase central venous pressure (CVP), decrease pulmonary artery (PA) pressure, resulting in obstructive shock. Smaller air bubbles obstruct pulmonary arterioles and microcirculation causing vasoconstriction and increasing pulmonary vascular resistance, PA pressure and RV pressure. In addition, venous air may leak through pulmonary capillaries into arterial circulation and cause arterial embolization and end organ ischemia.8
Incidence
It is estimated that the incidence of VAE with CVC placement is about 0.2%-1%. Interventional radiology literature suggests 0.13% in CVC placement while it is estimated that incidence in cardiac bypass surgery is between 0.003% and 0.007%. VAE are most common following otolaryngological and neurosurgical procedures, due to incisions being above the level of the heart at a distance greater than the CVP.4
Risk Factors1,2,7
- CV access, especially in situations of hypovolemia (decreased CVP)
- Pressurized infusions, including IV contrast injections for imaging
- Trauma (blunt or penetrating)
- Surgical: sitting craniotomy, spinal surgery, posterior fossa surgery, C-section, laparoscopic surgery (CO2 embolism)
Prevention of VAE 1,7,8
- Trendelenburg (head-down body tilt) position for placement & removal of internal jugular and subclavian CVC, while supine position for femoral CVC placement and removal.
- Positive-pressure mechanical ventilation reduces risk.
- Prepare and flush CVC prior to insertion, making sure no air bubbles remain in the catheter.
- Occlude the needle hub and/or catheter during insertion or removal.
- Keep all connections to the CVC closed when not being used.
- During removal, if the patient is following command, ask the patient to valsalva during expiration. Apply firm pressure for approximately 1 minute, without massaging site.
Clinical Manifestation
- Symptoms include acute onset dyspnea, cough, syncope, altered mental status and "mill wheel murmur" (which is specific but not sensitive).2,7
- Signs include hypoxia, hypotension, tachycardia.2,7
- Patients can exhibit signs of acute right-sided heart failure, cardiogenic shock (hypotension, oliguria, JVD) and acute embolic stroke (air bubbles pass through patent foramen ovale).8
It is a clinical diagnosis based on a high index of suspicion and exclusion of other life-threatening processes. Findings suggestive of VAE:
- End-tidal carbon dioxide (EtCO2) will fall due to increased physiological dead space and worsening V/Q mismatch.7
- EKG can show signs of right-heart strain (right axis deviation, RBBB, peaked P waves), non-specific ST changes and T-wave changes, ST depression or elevation consistent with acute myocardial ischemia or infarction.8
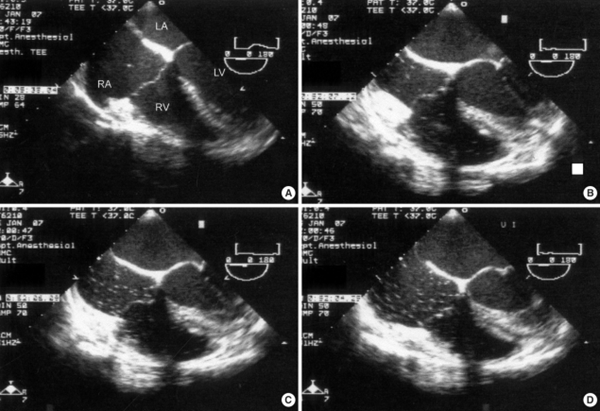
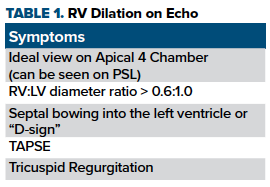
- Transthoracic Echocardiogram (TTE) or Transesophageal Echocardiogram (TEE) can show air in cardiac chambers, right ventricular dilation and dilated PA.6 RV:LV diameter ratio in a non-pathologic state should be 0.6:1.0. As right sided pressures start to exceed left sided pressures, you will get dilation of the RV and septal bowing into the left ventricle known as the "D-sign". On a more quantitative level, you can measure a tricuspid annular plane systolic excursion (TAPSE), which is a proxy for RV function, or tricuspid regurgitation, which will give you an estimate of mean pulmonary arterial pressure.
- Chest X-ray can show pulmonary edema8
- Elevated CVP, PA pressure8
Management Checklist1
- Ventilate at 100%O2 on ventilator or NRB. If hemodynamically unstable, intubate and consider increasing PEEP. These measures may speed air resorption however, they remain unproven.
- Place the patient in head down, left lateral decubitus to prevent air blocking RV outflow tract (unproven).
- Attempt to aspirate air from CVC.
- Chest compressions, again unproven but are thought to force air out of pulmonary outflow tract and break up large volumes of air in cardiac chambers.
- Increase IV fluids and add inotropic support if needed (epinephrine, norepinephrine, dobutamine).
- Hyperbaric oxygen for up to 6 hours once stabilized.
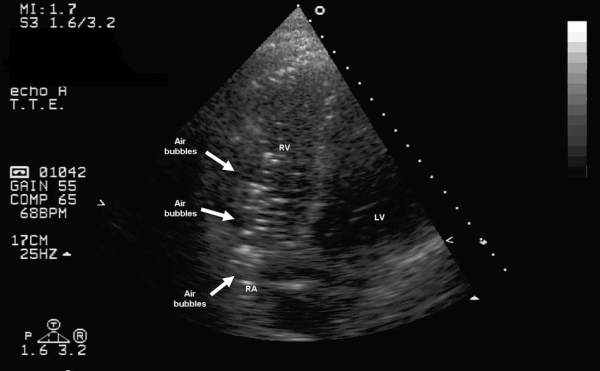
Figure 1. Massive air bubbles in RV 20 minutes after CVC removal. (image courtesy of Deceuninck et al.)

Figure 2. Dilation of the RV with RV:LV ratio >0.6:1.0
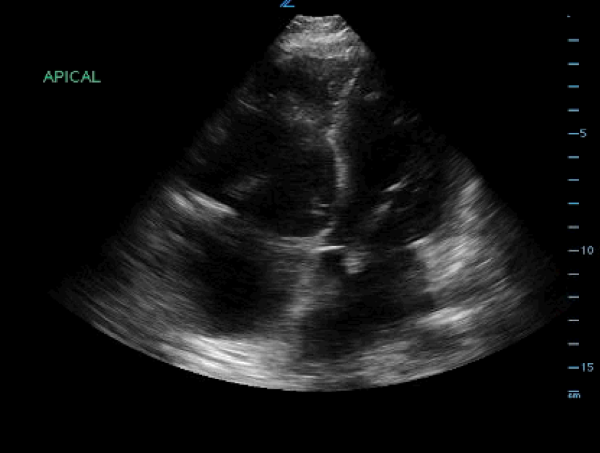
Figure 3. "D sign," septal bowing into the left ventricle
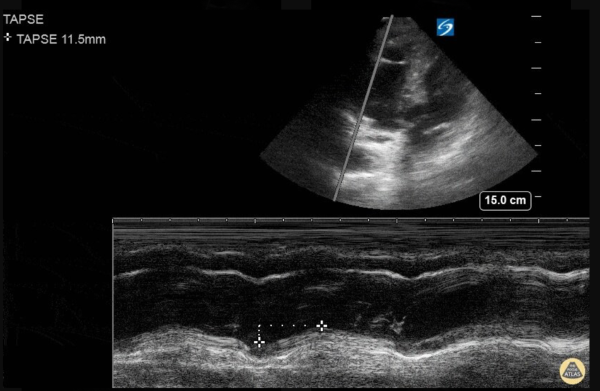
Figure 4. Tricuspid annular plane systolic excursion (TAPSE) measurement, which is a proxy for RV function. TAPSE can be measured by placing a cursor at the tricuspid lateral annulus and measuring the distance to systolic annular RV excursion. A distance of 17 mm or less is suggestive of RV strain. (Image courtesy of The Pocus Atlas)
Take-Home Points
- VAE is a rare but fatal complication of a common procedure in the ED and ICU.
- Prevention is key.
- Think of venous air embolism with sudden neurologic deterioration, hypotension, and hypoxia following CVC placement and surgery (especially neurosurgery).
- You cannot diagnose and treat something if you don’t think of it - keep broad differential.
References
- Borshoff DC, Lighthall G. The Anesthetic Crisis Manual. West Perth, W.A.: Leeuwin Press; 2013.
- Chuang DY, Sundararajan SA, Sundararajan VI, Feldman Dundefined, Xiong Wundefined. Accidental Air Embolism. Stroke. 2019;50(7). doi:10.1161/strokeaha.119.025340
- Deceuninck O, Roy LD, Moruzi S, Blommaert D. Massive Air Embolism After Central Venous Catheter Removal. Circulation. https://www.ahajournals.org/doi/abs/10.1161/circulationaha.107.701615. Published November 6, 2007. Accessed February 7, 2020.
- The Pocus Atlas (TPA). http://www.thepocusatlas.com/echocardiography-2.
- Gordy S, Rowell S. Vascular air embolism. International Journal of Critical Illness and Injury Science. 2013;3(1):73. doi:10.4103/2229-5151.109428
- Maddukuri P, Downey BC, Blander JA, Pandian NG, Patel AR. Echocardiographic Diagnosis of Air Embolism Associated with Central Venous Catheter Placement: Case Report and Review of the Literature. Echocardiography. 2006;23(4):315-318. doi:10.1111/j.1540-8175.2006.00211.x
- Marino PL. The ICU Book. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2014.
- O'Dowd LC, Kelley MA. Air embolism. UpToDate. https://www.uptodate.com/contents/air-embolism.