Case
A 16-year-old boy presents to the ED with right shoulder pain after strongly throwing a ball overhand. He denies any direct trauma or history of prior injury. On exam, he holds the affected shoulder in slight external rotation and abduction, with squaring of the shoulder contour. A hollow is appreciable beneath the posterior aspect of the acromion. The motor and sensory exams are intact to the five branches of the brachial plexus and distal pulses are strong. An attempt to range the shoulder is met with significant apprehension.
QUESTIONS
- How can you use point-of-care ultrasound (POCUS) to confirm your diagnosis?
- How can you use POCUS to provide analgesia?
- How can you use POCUS to confirm your therapy?
- Can POCUS eliminate pre- and postreduction radiographic assessments?
Anatomy
The glenohumeral (GH) joint is one of the largest joints of the body and has the greatest range of motion. It comprises three bones: the scapula, with its coracoid and acromion bony projections; the clavicle; and the humerus. The humerus articulates with the glenoid fossa of the scapula to form the GH joint. Due to its wide range of motion, the shoulder is the most commonly dislocated joint in the body, with anterior dislocations (as in the patient in this scenario) accounting for 95-97% of total dislocations. ¹ These can occur when large forces distract the humeral head from the inferior glenoid fossa, while the biceps and pectoralis muscles pull the humeral head anteriorly.
The Procedure
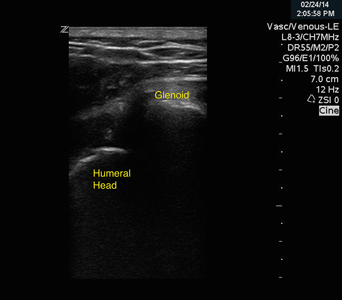
Plain radiography has been the historic modality for evaluating shoulder dislocation, but there may be a growing role for ultrasound (US) diagnosis. Recent evidence suggests that POCUS can confirm shoulder dislocation with improved sensitivity and efficiency relative to radiography. ² With the patient in a seated position and the indicator pointed to the patient's left, the high-frequency linear probe is placed in transverse orientation just below the scapular spine. In this orientation, the bony landmarks of the glenoid fossa and humeral head are identified. Bones reflect sound waves while their cortices cast deep shadows, causing them to appear as bright echogenic lines on ultrasound. In an anterior dislocation, the glenoid fossa will be empty, and the humeral head will be seen deep to the probe near the bottom of the screen (Image 1). Joint effusion or hemarthrosis may also be seen. Consider performing dynamic scanning by imaging a selected point between the humeral head and the glenoid and gently ranging the shoulder to confirm the expected absence of articulation.
Ultrasound may also aid successful reduction of the anterior dislocation. A recent meta-analysis suggested that intra-articular lidocaine provides equal pain control with fewer complications and greater first attempt success rates when compared to intravenous analgesia and sedation. ³ There appears to be a role for ultrasound-guided lidocaine placement as part of this procedure, though this technique has yet to be evaluated beyond case reports. ´
The posterior approach in GH joint injection is preferred because of the thin posterior joint capsule and the absence of significant neurovascular structures, bursae, and rotator cuff tendons. Placing the joint in slight flexion with mild distal inline traction may be useful. The acromion and coracoid processes should then be identified by following the scapular spine laterally until it turns anteriorly to become the acromion. The coracoid process should be identified below the lateral third of the clavicle.
Using aseptic technique, the skin should be prepared with betadine or chlorhexidine, and the foot of the US probe should be covered with a transparent dressing and sterile lubrication. Under long-axis visualization, a spinal needle can be inserted inferior to the posterior border of the acromion process . The tip of the needle should be aimed towards the coracoid process about 30 degrees medially, and advanced 2 to 3 cm. Once in the joint space, it is reasonable to aspirate to evaluate for and remove any hemarthrosis. Then, pushing slowly, confirmation of space expansion with injection of lidocaine can be confirmed on ultrasound.5 Generally, up to 15 cc of lidocaine can be placed into the joint space.
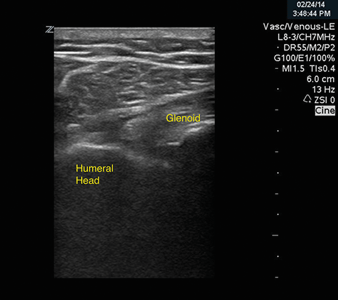
As always, after performing a reduction, the patient's neurovascular function should be assessed. Reexamination of the joint with ultrasound can confirm replacement of the humeral head into the glenoid fossa (Image 2). With mild internal and external rotation, the humeral head can be seen articulating with the glenoid. Immobilization should be performed with a sling and swath, with the shoulder placed in internal rotation and the elbow at 90 degrees.
Pearls, Pitfalls, and Further Discussion
A continued discussion on the utility of pre- and postreduction radiographs in the management of shoulder dislocation remains inconclusive. Ultrasound may provide an adjunct role, but its parameters have yet to be defined.6,7
Prereduction radiographs are typically obtained to confirm dislocation, type of dislocation, and presence of fracture. Several prospective trials selectively eliminated prereduction radiographs to demonstrate reduced time to reduction and reduced radiographic use without adverse events. The same studies also suggest both decreased patient discomfort and muscle spasm (which can result in a more difficult reduction).8-10 However, this selective practice is still not widely accepted. Although Hill-Sachs deformities, Bankart lesions, and greater tuberosity fractures generally do not alter the initial management of prompt closed reduction, high-energy injuries like humeral neck fracture-dislocations should be identified prior to determining an optimal reduction strategy. Also, attempting an anterior closed reduction technique on a non-dislocated, or posteriorly dislocated, shoulder can be harmful. Some authors suggest obtaining US views of the humeral head, neck, and shaft to exclude obvious fracture, but this practice has yet to be established. ¹ ¹
Postreduction radiographs are typically obtained to confirm successful reduction and to evaluate for presence of any fractures sustained either iatrogenically or not initially visualized on the prereduction radiograph. Iatrogenic fractures as the result of shoulder reduction remain a rare event.12 Small prospective, observational studies show that a significant number of associated fractures were not appreciable until the postreduction radiograph, but no injury was clinically significant in terms of changing subsequent emergency department management. It is uncertain what role ultrasound may have in evaluating for postreduction fractures.
Conclusion
Ultrasound may have a future role in safely omitting prereduction and postreduction radiographs, but its optimal application is currently in point-of-care confirmation of successful closed reduction, with some role in shoulder injection. This likely avoids readministration of analgesia in a patient requiring multiple reduction attempts, expedites overall care, and can reduce costs and radiation exposure.
REFERENCES
- Marx, J et al. Rosen's Emergency Medicine: Concepts and Clinical Practice. Mosby Elsevier. Philadelphia: 2010.
- Abbasi S, et al. Diagnostic accuracy of ultrasonographic examination in the management of shoulder dislocation in the emergency department. Annals of Emergency Medicine. 2013;62(2):170-5.
- Jiang N, et al. Intra-articular lidocaine versus intravenous analgesia and sedation for manual closed reduction of acute anterior shoulder dislocation: an updated meta-analysis. J Clin Anesth. 2014;26(5):350-9.
- Breslin K, et al. Ultrasound-guided intra-articular lidocaine block for reduction of anterior shoulder dislocation in the pediatric emergency department. J.Pediatr Emerg Care. 2014;30(3):217-20.
- Reichman EF. Emergency Medicine Procedures, 2e. McGraw Hill Education. New York: 2013.
- Blakeley CJ, et al. A novel use of portable ultrasound in the management of shoulder dislocation. Emerg Med J. 2009;26(9):662-663.
- Halberg MJ, et al. Bedside ultrasound for veriï¬cation of shoulder reduction. Am J Emerg Med. 2009;27:134.e5-134.e6.
- Shuster M, et al. Prospective evaluation of a guideline for the selective elimination of pre-reduction radiographs in clinically obvious anterior shoulder dislocation. CJEM. 2002;4(4):257-62.
- Shuster M, et al. Prereduction radiographs in clinically evident anterior shoulder dislocation. Am J Emerg Med 1999;17(7):653-8.
- Hendey GW, et al. Selective radiography in 100 patients with suspected shoulder dislocation. J Emerg Med. 2006;31(1):23-8.
- Yuen CK, et al. Ultrasound diagnosis of anterior shoulder dislocation Hong Kong J Emerg Med. 2009;16(1):29-34.
- Kahn JH, Mehta SD. The role of post-reduction radiographs after shoulder dislocation. J Emerg Med. 2007;33(2):169-73.