Cardiac arrest is one of the most demanding presentations for emergency physicians to manage, due to its diagnostic uncertainty and time-sensitive complications.
High-quality chest compressions have been shown to increase survival and improve neurological outcomes.1 Focused transthoracic echocardiography (TTE) can identify critical, potentially reversible, pathology during cardiac arrest: tension pneumothorax, cardiac tamponade and hypovolemia.2,3 However, TTE results in prolonged chest compression pauses5 and may compromise high-quality CPR. TTE is also limited by impediments to images generated through the skin surface, such as defibrillation pads, body habitus, and gastric air. Focused transesophageal echocardiography (TEE) has emerged as an alternative to TTE that overcomes these limitations and has the added benefit of improving, rather than hindering, the delivery of chest compressions.5
Advantages
The transducer used in TEE is inserted into the esophagus and allows for visualization of clots in transit, clots in the pulmonary arteries, aortic dissections and cardiac tamponade. TEE permits the optimization of real-time chest compressions relative to cardiac anatomy, which is particularly useful for people whose left ventricle, the target of chest compressions, is not located beneath the sternum. For example, radiologic studies have found that the left ventricular outflow tract, aortic root or aortic valve are located beneath the center of the sternum in 50% to 80% of patients. Therefore, TEE-directed modifications could be used to optimize cerebral perfusion.5,6 TEE can also be used during post-arrest care for procedural guidance, including extracorporeal life support and placement of a temporary pacemaker.5
Risks
The safety of TEE in cardiac arrest has not been studied directly, so the complications can only be deduced from ambulatory TEE examinations. Major complications such as oropharyngeal trauma, esophageal perforation and major bleeding events are rare with incidences reported as less than 1%. Additionally, since TEE can obtain life-saving information without compromising high-quality CPR, the risk-benefit ratio for TEE in cardiac arrest is extremely favorable.5
Practicality and Value
In a resuscitative setting, TEE occurs after endotracheal intubation.5 TEE transducers require specific storage and cannot stay with the machine, so it is recommended to designate an easily accessible storage location.5 A recent study focused on TEE in ED cardiac arrest found that is was achievable to perform a focused TEE exam early in resuscitation and that TEE had a therapeutic or prognostic impact in 97% of the cases.8-11
Imaging Protocol
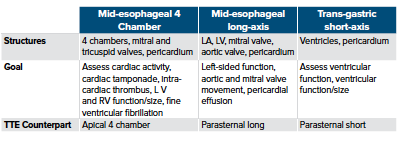
The American College of Emergency Physicians (ACEP) published a three-view (mid-esophageal 4-chamber, mid-esophageal long-axis, and transgastric short-axis views), goal-directed protocol for TEE in cardiac arrest, which represents the minimum standard-of-care.9 The protocol was designed with an appreciation for the scope of ED echocardiography and emphasizes efficiency, redundancy, and views that are anatomically like familiar TTE views.9
A recent prospective observational study consisting of thirty-three patients presenting to the ED with out-of-hospital cardiac arrest used a four-view protocol for post-intubation TEE during cardiac arrest.11 TEE was used to assist with diagnostic uncertainty, evaluate cardiac activity and determine CPR quality through AMC assessment. All participating physicians completed standardized training consisting of at least 8 hours of didactics, high-fidelity simulation, and a minimum of 10 proctored examinations.11
The four-view protocol was obtained in 100% of cases, with an average ED door to TEE time of 12 minutes, which supports the feasibility of TEE in the setting of cardiac arrest.11 TEE was found to have a diagnostic, therapeutic or prognostic impact in 97% of cases. Per this protocol, a mid-esophageal bicaval view was obtained in addition to the three-views suggested by ACEP. The authors report that this view aided with the initiation of extracorporeal life support in 21% of cases, which suggest that best practices for TEE during cardiac arrest may consist of a four-view protocol, like the one provided in this study.11
Future Work
For TEE to become a widespread practice throughout emergency departments in the United States, future work is needed to assess its impact on patient outcomes, cost-effectiveness and to ensure resources are available for providers to meet training requirements. The main use of TEE in the ED has been cardiac arrest, but indications will likely expand to include intubated, septic patients and patients requiring hemodynamic monitoring.
References
- Nolan J, Ornato J, Parr M, Perkins G, Soar J. Resuscitation highlights in 2014. Resuscitation 2015;89:A1–6.
- Gaspari R, Weekes A, Adhikari S. Emergency department point-of-care ultrasound in out-of-hospital and in-ED cardiac arrest. Resuscitation 2016;109:33–9. 10. Nolan J, Ornato
- Labovitz AJ, Noble VE, Bierig M.Focused cardiac ultrasound in the emergent setting: a consensus statement of the American society of Echocardiography and American College of Emergency Physicians.
- Clattenburg EJ, Wroe P, Brown S. Point-of-care ultrasound use in patients with cardiac arrest is associated prolonged cardiopulmonary resuscitation pauses: a prospective cohort study. Resuscitation 2018;122:65 –8.
- Teran F, Prats M, Nelson B, et. al (2020, August 11). Focused Transesophageal Echocardiography During Cardia Arrest Resuscitation. Retrieved October 14, 2020, from https://www.onlinejacc.org/content/76/6/745
- Nestaas S, Stensæth KH, Rosseland V, Kramer-Johansen J. Radiological assessment of chest compression point and achievable compression depth in cardiac patients. Scan J Trauma Resus Emerg Med. 2016;24:54.
- Hwang SO, Zhao PG, Choi HJ. Compression of the left ventricular outflow tract during cardiopulmonary resuscitation. Acad Emerg Med. 2009;16:1–8.
- Arntfield R, Pace J, McLeod S. Focused transesophageal echocardiography for emergency physicians—description and results from simulation training of a structured four-view examination. Crit Ultrasound J. 2015;7:27.
- Fair J, Mallin M, Mallemat H, et.al Transesophageal Echocardiography: Guidelines for Point-of-Care Applications in Cardiac Arrest Resuscitation. Ann Emerg Med. 2018;71(2):201-207.
- Arntfield R, Pace J, McLeod S, et al. Focused transesophageal echocardiography for emergency physicians-description and results from simulation training of a structured four-view examination. Crit Ultrasound J. 2015;7(1):27.
- Teran F, Dean AJ, Centeno C, et al. Evaluation of out-of-hospital cardiac arrest using transesophageal echocardiography in the emergency department. Resuscitation. 2019;137:140-147.



