Sarah Espinoza, MD, Resident Physician, UC San Diego, San Diego, CA
Background: Perilunate dislocation with transcaphoid fracture
Lunate and perilunate dislocations are a relative spectrum of similar high- energy traumatic injuries of the wrist and hand. They are often associated with other injuries or fractures of the carpal bones or the distal radius. As individual entities, lunate and perilunate dislocations can be easily confused with each other. The difference lies in the lunate's position relative to the distal radius. In a true lunate dislocation, the lunate alone is dislodged from its position, while the rest of the carpal bones remain intact and are aligned longitudinally with the diaphysis of the radius. A perilunate dislocation indicates that the lunate bone has retained it positioning and alignment, whereas the other carpal bones have slipped in relation to the radius, typically dorsally.
The incidence of scaphoid fractures is about 1 in 100,000 people per year.1 Perilunate dislocations, lunate dislocations, and perilunate fracture dislocations have been estimated to comprise less than 10% of all wrist injuries. 61% of these were of the perilunate transcaphoid type (perilunate dislocation with transverse scaphoid fracture). One study suggests 0.5-6.5% of all carpal fractures are of this same type.2 Perilunate dislocations are relatively rare, but commonly have an associated scaphoid fracture or occasionally an ulnar styloid fracture.3 However, the true incidence of perilunate and lunate dislocations is unknown. It is believed that many go undiagnosed because their radiographic findings can be very subtle, and often are not fully appreciated.4 It is estimated that up to 25% of these injuries are diagnosed late.5 It is important for emergency medicine physicians to be able to recognize these injuries, especially when there is a scaphoid fracture present, as this can be a visually distracting injury on radiographs.
The transcaphoid perilunate dislocation combination is more unstable than an isolated scaphoid fracture due to the ligamentous damage that occurs with the perilunate dislocation.6 Anatomically, the mechanism of lunate dislocation involves progressive ligamentous injury, starting with rupture of the radioscaphocapitate and scapholunate ligaments, leading to a capitolunate dislocation. The lunotriquetral ligament is then disrupted; this allows the lunate to dislocate from its carpal space.4
The Mayfield classification system recognizes the similar nature of lunate and periluante injuries and attempts to categorize them into four stages. Stage 1 is the scapholunate dislocation, Stage 2 involves disruption of the lunocapitate, Stage 3 is the typical perilunate dislocation, and Stage 4 is complete dislocation of the lunate from its fossa.
Diagnosis
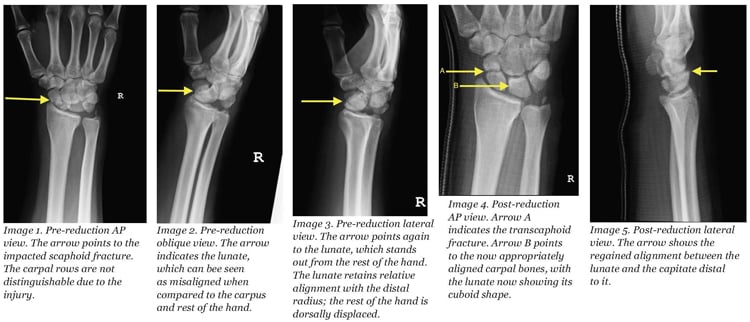
History and exam are pertinent to making the diagnosis. Swelling over the dorsum of the hand with tenderness to palpation over the mid-carpus may tip off the clinician. In lunate dislocations there is frequently some degree of median nerve compression injury, so loss of sensation in this nerve's distribution, or loss of thumb abduction or flexion may also be an indicator. However, x-rays are going to be most important in making the final diagnosis. Given that these injuries are under-diagnosed, it is important to have a systematic approach for reading radiographs. In perilunate dislocation injuries, as seen in the patient in this scenario, the lunate will often appear triangular instead of cuboid on an AP view. On the lateral view, the lunate rotates forward and all the other carpal bones are dislocated posteriorly with respect to the lunate.3 Remembering that the carpal bones should align longitudinally with the radius can also help in radiographic diagnosis.
Treatment
Perilunate dislocations require reduction at the time of the initial injury. Further treatment is dictated by the degree of injury, and is often done as an outpatient. The type of immobilization is determined by the presence of a scaphoid fracture. While isolated scaphoid fracures are typically treated with either a short- or long-arm thumb spica splint (depending on if it is a distal or proximal fracture), perilunate fracture dislocations require either a long-arm or a double sugar-tong splint to include spica, if the scaphoid is injured.5 Immobilization time may be dictated by the location of the scaphoid fracture: 4-6 weeks for distal, 10-12 for mid-body, and 12-20 for proximal.
Hand surgery follow up is required if surgeons are not immediately involved with this case in the emergency department, as many of these patients will ultimately need surgical treatment. The need for surgery or surgical reduction greatly increases with time from initial injury to first diagnosis. Late reduction is almost impossible. The patient may require multiple surgeries with extensive dissection, and possibly proximal row carpectomy if not promptly diagnosed. Emergent surgical intervention is required in the case of open injuries or in signs of progressive median nerve dysfunction.5
Conclusion
As previously mentioned, this fracture pattern is often missed on initial evaluation and can lead to devastating complications. Prognosis is improved with early reduction. Complications include a missed injury, median nerve damage, varied degree of impaired function, lunate osteonecrosis (Kienbock's disease), chondrolysis, complex regional pain syndrome, carpal instability, scaphoid nonunion or malunion, and early arthritis. Avascular necrosis of the scaphoid is relatively common due to its distal to proximal blood flow, but it can also occur in the lunate despite its dual arterial blood supply from the volar and dorsal aspect of the bone. Early proper management is necessary to help prevent this complication. For associated scaphoid fractures, the degree of displacement of this bone increases the incidence of non-union and avascular necrosis. Even with early proper treatment, post-traumatic arthritis occurs in 56% of patients within an average of 6.25 years. Patients may also develop decreased grip strength, decreased range of motion, and persistent pain.5
The presented case scenario should stress the importance of not only identifying the scaphoid injury, but also doing a thorough read of the x-ray ensuring there is no associated perilunate dislocation. There is significant morbidity associated with a miss. Most of these cases will come through the emergency department, and it is up to us as physicians to be thorough and correctly manage this injury pattern.
- Tassel, D., Owens, B., Wolf, J. Incidence Estimates and demographics of Scaphoid fracture in the U.S. Population. The Journal of Hand Surgery. Vol 35, Issue 8, August 2012, 1242-1245.
- Burroughs, K, MD. Scaphoid and Lunate Fractures. Uptodate.com. Nov 2012.
- www.learning radiology.com/notes/bonenotes/perlunatedislocatepage
- emedicine.medscape.com/article/1240108-overview
- Garg B; Goyal, T; Kotwal, P. Staged reduction of neglected transscaphoid perilunate fracture dislocation: A report of 16 cases. J Orthop Surg Res. 2012; 7:19.
- www.wheelessonline.com/ortho/perilunate_dislocations
- Kardashain, G, MD; Christoforou, D, MD; Lee, S, MD. Perilunate dislocations. Bulletin of the NYU hospital for Joint Diseases 2011; 69(1):87-96.