The need for a central line is commonplace in the emergency department and critical care units.
When deciding which of the three typical sites (internal jugular, femoral, and subclavian) to choose for central venous access, much can go into the site selection. Infection rates, risk of bleeding, risk to surrounding structures, incidence of deep venous thrombosis (DVT), and specific complications such as pneumothorax are all things to consider. Often logistical concerns can contribute to our choice as well. Is a C-collar in place? Are the endotracheal tube straps in the way? Is there an overlying cellulitis of the groin? Will a large pannus make a femoral approach difficult? Is this line emergent and is an ultrasound readily available? Does the patient already have a pneumothorax or chest tube? Suffice to say, there are many reasons a site may or may not be ideal — so it is good to have choices.
Is there a “best” site? Looking at some retrospective studies and meta-analyses, there is a suggestion that the internal jugular (IJ) is by far the most common site for central venous cannulation.1,2 Interns and medical students are often taught that the femoral site has higher rates of infections, and the subclavian is technically difficult and risks the development of a pneumothorax. Is this what the evidence shows? Why does the CDC recommend the subclavian site as the site of choice for temporary non-tunneled central lines,3 and why don’t we follow this advice?
The randomized controlled trial, 3SITES, compared femoral vs internal jugular vs subclavian venous access, with the primary outcome being a composite of blood stream infection and DVT. Interestingly, the subclavian site was significantly better when compared to both the IJ and femoral sites for this outcome. Mechanical complications were treated as a composite as well, and included pneumothorax, arterial injury, and hematoma. These complications did occur more frequently for the subclavian site when compared to both other sites. This was significantly more than the femoral site but not statistically significant when compared to the IJ. Pneumothorax accounted for most of the mechanical complications with occurrences of 1.5% (subclavian), 0.5% (IJ), and 0% (femoral). Of note, ultrasound guidance was not protocolized for this trial, a significant number of the lines were placed by landmark technique, and the analysis showed an interaction between mechanical complications and not using ultrasound.4
So, can ultrasound reduce the feared mechanical complications of the subclavian site? A 2011 randomized controlled trial compared just this: landmark vs ultrasound-guided subclavian central catheter placement. Pneumothorax occurred 4.9% of the time in the landmark group and zero times in the ultrasound group.5
These results are obviously impressive and prompt a close look at the description of their technique (important to note: all providers had >6 years’ experience in central line placement). The study included four key steps that may have contributed to the few mechanical complications experienced:
- Ultrasound evaluation of the ipsilateral and contralateral subclavian and axillary veins, both with infraclavicular and supraclavicular approaches looking for anatomic findings which may portend difficult placement.
- A high frequency linear probe was used to find an area of the subclavian (or sometimes axillary) vein in long axis (more on axis choice later) that was amenable to catheterization and that passed over a thoracic rib.
- Under real-time direct visualization, the needle was advanced directly at the venous portion overlying a thoracic rib with the idea that the rib would protect from posterior wall sticks.
- Ultrasound was used to confirm wire placement and investigate the ipsilateral IJ and contralateral subclavian vein in attempt to diagnose misplaced wires prior to catheter placement.5
Figure 1. Long axis scan of right subclavian anatomy showing subclavian vein=SV, cephalic vein=CV, axillary vein=AV, and an underlying thoracic rib.
The use of a thoracic rib (the second rib typically) as protection against posterior wall injury and subsequently pleural injury with potential for pneumothorax has been described elsewhere — specifically in a paper dubbing it the Pleural Avoidance and Rib Technique (PART) method. In that paper, the authors described 76 attempts at subclavian catheter placement under ultrasound guidance and reported a 100% success rate of catheter placement with zero pneumothoraces or pleural injuries.6
It may be difficult occasionally to find a suitable target overlying the second rib. The shrug technique is a theoretical technique in which the patient's shoulders are shrugged upwards, thereby displacing the clavicles cranially and potentially opening a new window where the subclavian vein overlies the first rib. This similar technique as described above can be employed to protect the pleura.7
Figure 2. Shrugging the shoulders can alter the anatomy, opening new windows or pushing the subclavian vein to overly a thoracic rib.
Other things to consider: which side to choose and even which ultrasound axis to use. When compared, right-sided subclavian attempted catheter placements are associated with significantly more misplaced catheters than left-sided attempts (9.6% vs 0%).8 Short axis ultrasound technique has been shown to have significantly better first attempt success, shorter duration of procedure, and fewer complications when compared to long axis technique.9
Technique
Putting this all together: Investigate all central line sites with a physical exam and under ultrasound.
If no contraindication exists and the subclavian is determined to be the safest site, preferentially prepare for a left subclavian approach. Position and prepare the patient in a standard fashion for central line placement — in the Trendelenburg position, sterilely prepped and draped, etc. Use standard central line kits, typically a 20cm catheter length for multi-lumen catheters, but sometimes shorter depending on patient size or vascular access point. Using a high-frequency linear probe optimized for near-to-mid field resolution, scan in short and long axis to find the course of the subclavian vein or proximal axillary vein. Then find the portion that passes over a thoracic rib and that is free from other vascular structures or nerves in the path of the catheter. Confirm the vessel with typical compression and doppler techniques.
Figure 3. Doppler evaluation of the right subclavian vein to confirm venous tracing.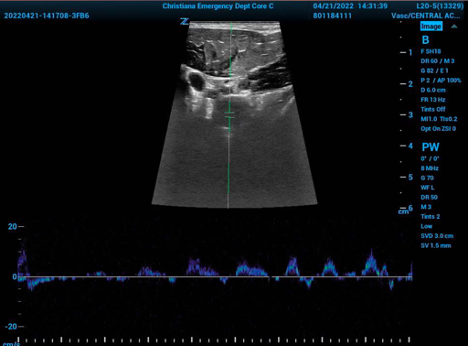
If there is no accessible portion overlying a thoracic rib, place the patient's shoulders in a shrugged position and re-evaluate. Identify the pleural edge and know its location to avoid it going forward.
Figure 4. Left subclavicular anatomy with pleura in view. SV=subclavian vein, SA=subclavian artery. 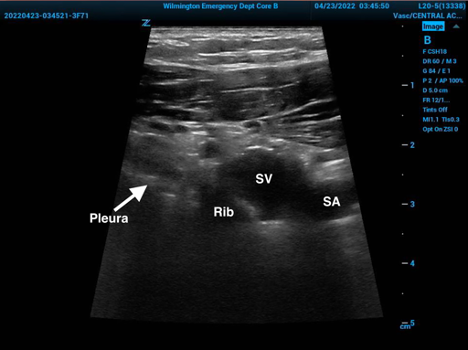
Under direct visualization, direct the needle in short axis view until venous access is accomplished and then continue with the standard Seldinger technique. Confirm wire placement with ultrasound and ask an assistant to scan the ipsilateral IJ and contralateral subclavian investigating for wire malposition while maintaining site sterility. Complete the rest of the standard catheter placement procedure and catheter position confirmation.
A subclavian approach should be considered for every patient undergoing central venous catheterization, but it is not always the correct site to choose. In addition to lower infections, the 3SITES trial also showed it was the best site in regard to minimizing DVTs.4 An experienced provider, or a provider under this supervision, can combine practice, experience, and pearls from the data above to improve the success of subclavian venous catheter placement and minimize the complications significantly. Using the short axis view, choosing the left side, directing the needle at a protecting thoracic rib (with or without the shrug technique) can all improve complication rates and procedural success. 3SITES was not designed to give definitive advice for which site is best, is limited in its generalizability to present day due to lack of a requirement for ultrasound use, but when combined with the other evidence above, suggests that the widespread use of ultrasound should perhaps reorder how we rank central line sites.
It bears repeating, provider experience and comfort are of great importance and likely factor heavily into the success and lack of complications seen in the above trials. Patient factors are also important to consider; a patient who is difficult to ventilate and/or oxygenate will not tolerate the development of a pneumothorax. Subclavian catheters are also relatively contraindicated in patients at risk for permanent renal failure due to concern for development of subclavian stenosis, which would complicate hemodialysis options. The subclavian site is also not easily compressed and may pose higher risk in patients with a bleeding diathesis. By no means is this an exhaustive list of considerations. That being said, it is good to have choices, and there are patients in whom an IJ or femoral approach are not possible or pose unacceptably high risk.
References
- Bell J, Goyal M, Long S, et al. Anatomic Site-Specific Complication Rates for Central Venous Catheter Insertions. J Intensive Care Med. 2020;35(9):869-874.
- Björkander M, Bentzer P, Schött U, Broman ME, Kander T. Mechanical complications of central venous catheter insertions: A retrospective multicenter study of incidence and risks. Acta Anaesthesiol Scand. 2019;63(1):61-68.
- Guidelines for the Prevention of Intravascular Catheter-Related Infections. Centers for Disease Control and Prevention. 2011.
- Parienti JJ, Mongardon N, Mégarbane B, et al; 3SITES Study Group. Intravascular Complications of Central Venous Catheterization by Insertion Site. N Engl J Med. 2015 Sep 24;373(13):1220-1229.
- Fragou M, Gravvanis A, Dimitriou V, et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med. 2011;39(7):1607-12.
- Senussi MH, Kantamneni PC, Omranian A, et al. Revisiting Ultrasound-Guided Subclavian/Axillary Vein Cannulations: Importance of Pleural Avoidance With Rib Trajectory. J Intensive Care Med. 2017;32(6):396-399.
- Farkas J. (2018, April 23). PulmCrit- Shrug Technique for US-guided subclavian lines. Retrieved April 22, 2022.
- Tarbiat M, Manafi B, Davoudi M, Totonchi Z. Comparison of the Complications between Left Side and Right Side Subclavian Vein Catheter Placement in Patients Undergoing Coronary Artery Bypass Graft Surgery. J Cardiovasc Thorac Res. 2014;6(3):147-51.
- Vezzani A, Manca T, Brusasco C, et al. A randomized clinical trial of ultrasound-guided infra-clavicular cannulation of the subclavian vein in cardiac surgical patients: short-axis versus long-axis approach. Intensive Care Med. 2017;43(11):1594-1601.



