Stellate ganglion blockade has been used for over a century to decrease sympathetic tone to the heart.
The left cardiac sympathetic denervation surgical procedure was first performed in 1916 to treat angina, severing the sympathetic innervation of the heart.1 This surgical sympathetic denervation of the heart was later shown to reduce the incidence of ventricular fibrillation, specifically in animal studies.2 A percutaneous procedure was developed in 1971 to interrupt sympathetic stimulation to the heart; the stellate ganglion block (SGB).3 The procedure involves injecting local anesthetic to the stellate ganglion. The SGB is most commonly used in the setting of electrical storm: 3 or more episodes of sustained ventricular arrhythmia over 24 hours.4 While the SGB has been documented as a treatment option for refractory ventricular arrhythmias, its use in the emergency management of pulseless arrest with shockable rhythm has not been well described.
Case Report
A 74-year-old man presented to the emergency department via Emergency Medical Services (EMS) in cardiac arrest. The patient had a reported history of hypertension and previous myocardial infarction with stenting in 2000. The patient had been playing blackjack at a casino and started having seizure-like activity. A bystander, who happened to be a nurse, was unable to find a pulse and initiated CPR reportedly within one minute of symptom onset. EMS arrived within 7 minutes. They placed a defibrillator and a mechanical compression device. EMS noticed him to be in ventricular fibrillation. He was defibrillated unsuccessfully with 200 joules. The patient was then intubated with a 7.5 endotracheal tube. Advanced Cardiac Life Support (ACLS) was continued and the patient was defibrillated three more times en route to the ED. With EMS, the patient was given epinephrine 3 times and amiodarone 300 mg once.
The patient arrived to the emergency department 25 minutes after his initial electrical event. Correct placement of the endotracheal tube was verified. The mechanical compression device was continued. The patient was placed on a Zoll defibrillator with anterior-posterior pad placement. He arrived with a right humeral intraosseous line. A second right tibial intraosseous line and right femoral central line were placed. Throughout the remainder of the patient’s resuscitation the ACLS algorithm was followed with epinephrine every 3-5 minutes and pulse checks continued every 2 minutes.
After one initial 200 joule defibrillation was unsuccessful a second set of defibrillation pads were placed in the anterior-lateral position. The patient remained in refractory ventricular fibrillation and he was defibrillated using dual sequential defibrillation with each machine delivering 200 joules, which was unsuccessful. The remaining defibrillations were dual sequential defibrillations. During the following rounds of ACLS the patient was given adjunct medications including calcium, bicarbonate, magnesium and a dose of 150 mg amiodarone.
At this point the patient had been defibrillated with 200 joules four times and had dual-sequential defibrillation with a total of 400 joules two times. The patient was then given lidocaine 100 mg IV, esmolol 4,535 mcg (500 mcg/kg) and an infusion of esmolol 100 mc/kg/minute was initiated afterwards. He remained in ventricular fibrillation.
ACLS was continued with defibrillation and epinephrine per ACLS guidelines. The patient remained in refractory ventricular fibrillation. At this point a stellate ganglion block was performed with ongoing CPR. The stellate ganglion was localized using ultrasound at the level of C4/C5. A total of 5 cc of 2% lidocaine was injected. At pulse check the patient remained in ventricular fibrillation. He was defibrillated with dual sequential defibrillation and at pulse check he had palpable radial pulses.
The patient had a total downtime of approximately 45 minutes. Aggressive resuscitative measures were taken, as the patient had bystander CPR immediately initiated by a trained medical professional. The patient also had a shockable rhythm during resuscitation, which encouraged the medical team to continue efforts.
Discussion
It is understood that ventricular arrhythmias are initiated by myocardial injury. Cardiac myocytes damaged from infarction become arrhythmogenic. This reduced threshold for arrhythmia and an increase in catecholamines with increased sympathetic nervous system activity creates ventricular arrhythmias that are difficult to treat.5 The surge of catecholamines caused by the increased sympathetic drive leads to release of endogenous epinephrine, which is inherently arrhythmogenic. This arrhythmogenicity is compounded by exogenous epinephrine given during ACLS resuscitative efforts. Esmolol has been described to help create a sympathetic blockade, terminating arrhythmias induced by hyper-sympathetic states.6 A fascial plane block of the stellate ganglion may also terminate otherwise intractable sympathetic activity. In this case report, we describe the use of the stellate ganglion block during cardiac arrest due to refractory ventricular fibrillation.
The sympathetic nervous fibers that innervate the head, neck, heart and upper limbs ascend from the first thoracic segments through the sympathetic chain to the superior, middle and inferior cervical ganglions.7 The stellate ganglion is composed of the fusion between the inferior cervical ganglion and the first thoracic ganglion. Its location is described as posterior to the carotid artery and between C5 and T1.8,9 Local anesthetic is instilled under the prevertebral fascia at that level allowing the anesthetic to be distributed to the stellate ganglion. There is evidence that the left stellate ganglion is preferential to the right stellate ganglion in providing sympathetic blockade to the heart, making the left SGB the ideal target for blockade.8
Procedural Tips
ED access to ultrasound with linear transducer capabilities is nearly ubiquitous. The procedure for SGB has come to include ultrasound guided techniques, making the procedure safely accessible to most emergency departments.10
- A linear transducer is oriented transverse on the left anterior neck perpendicular to the trachea.
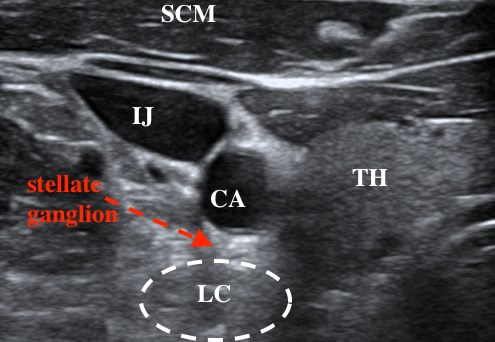
- The probe should be moved lateral for adequate visualization of the carotid artery, vertebral body of C6 or C7 and the longus colli muscle (figure 1). Figure 1. Nomenclature: SCM—sternocleidomastoid; TH—thyroid; LC—longus coli; IJ—internal jugular ; CA—carotid artery
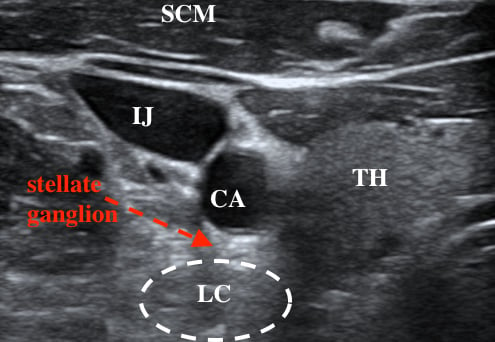
- A needle is then inserted and directed posterior to the carotid artery and superficial to the longus coli just deep to the prevertebral fascia. A 2 cm needle is sufficient.
- Lidocaine should slowly be injected and observed on ultrasound to separate the muscle and fascial layers as confirmation of correct placement. In this case report a total of 10 mL of 1% lidocaine was instilled to create a temporary blockade of sympathetic activity. Bupivacaine is commonly used in the anesthesia literature at 0.25 to 0.5% at a volume up to 9 mL.11 Lidocaine 2% of 8 mL has also been described and is effective, although the procedure can also be done successfully with similar volume doses of lidocaine 1%.12
In our case, the arrhythmia did not terminate immediately after the lidocaine was instilled. The arrhythmia persisted for another 2 minutes, approximately, during which ACLS was continued. This delay in arrhythmia cessation suggests that the decreased sympathetic tone ultimately terminated the arrhythmia.
Further Study
The efficacy of the SGB in the setting of cardiac arrest due to ventricular arrhythmias is not well documented or understood. There have been case reports in cardiology, anesthesia, and only recently, emergency medicine.13-16 The emergent nature and rarity of cardiac arrest caused by ventricular arrhythmia makes it difficult to create effective studies about this subject. Margus et al. note in their case report that the American Heart Association and American College of Cardiology guidelines for the treatment of ventricular arrhythmias state that "the significant morbidity and limited options in these patients make cardiac sympathetic denervation a reasonable option."13 The SGB is a relatively simple procedure that is minimally invasive. In cases of ventricular arrhythmias causing cardiac arrest this procedure can be utilized as an attempt at resuscitation.
Case Conclusion
EKG was obtained shortly after ROSC and showed a left bundle branch block meeting Sgarbossa criteria. Cardiology was called, and the catheterization laboratory was activated. The patient had a 100% right circumflex lesion, 70% left anterior descending stenosis, and 40% left circumflex lesion. Over the course of the next 24 hours the patient did not have meaningful recovery. Family decided to withdraw care.
TAKE-HOME POINTS
- The ultrasound-guided stellate ganglion block may be used as an adjunct to established methods during pulseless ventricular arrhythmias.
- It is a potentially lifesaving procedure that is within the emergency physician’s scope of practice.
References
- Driver BE, Debaty G, Plummer DW, Smith SW. Use of esmolol after failure of standard cardiopulmonary resuscitation to treat patients with refractory ventricular fibrillation. Resuscitation. 2014;85(10):1337-1341.
- Margus C, Correa A, Cheung W, et al. Stellate Ganglion Nerve Block by Point-of-Care Ultrasonography for Treatment of Refractory Infarction-Induced Ventricular Fibrillation. Ann Emerg Med. 2020;75(2):257-260.
- Piraccini E, Munakomi S, Chang KV. Stellate Ganglion Blocks. [Updated 2021 Feb 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507798/
- Aliot EM, Stevenson WG, Almendral-Garrote JM, et al. EHRA/HRS Expert Consensus on Catheter Ablation of Ventricular Arrhythmias: developed in a partnership with the European Heart Rhythm Association (EHRA), a Registered Branch of the European Society of Cardiology (ESC), and the Heart Rhythm Society (HRS); in collaboration with the American College of Cardiology (ACC) and the American Heart Association (AHA). Heart Rhythm. 2009;6(6):886-933.
- HARRIS AS, ESTANDIA A, TILLOTSON RF. Ventricular ectopic rhythms and ventricular fibrillation following cardiac sympathectomy and coronary occlusion. Am J Physiol. 1951;165(3):505-512.
- Chang, J. H., & Song, S. O. (2001). Minimal Concentration of Lidocaine for a Diagnostic
Stellate Ganglion Block. Korean Journal of Anesthesiology, 41(2), 165. https://doi.org/10.4097/kjae.2001.41.2.165 - Hayase J, Patel J, Narayan SM, Krummen DE. Percutaneous stellate ganglion block suppressing VT and VF in a patient refractory to VT ablation. J Cardiovasc Electrophysiol. 2013;24(8):926-928. doi:10.1111/jce.12138
- Meng L, Tseng CH, Shivkumar K, Ajijola O. Efficacy of Stellate Ganglion Blockade in Managing Electrical Storm: A Systematic Review. JACC Clin Electrophysiol. 2017;3(9):942-949. doi:10.1016/j.jacep.2017.06.006
- Biagini A, Sabino F, Paladini G, et al. Treatment of perinfarction recurrent ventricular fibrillation by percutaneous pharmacological block of left stellate ganglion. Clin Cardiol. 1985;8(2):111-113. doi:10.1002/clc.4960080209
- Moss AJ, McDonald J. Unilateral cervicothoracic sympathetic ganglionectomy for the treatment of long QT interval syndrome. N Engl J Med. 1971;285(16):903-904. doi:10.1056/NEJM197110142851607
- Nademanee K, Taylor R, Bailey WE, Rieders DE, Kosar EM. Treating electrical storm : sympathetic blockade versus advanced cardiac life support-guided therapy. Circulation. 2000;102(7):742-747. doi:10.1161/01.cir.102.7.742
- Schwartz PJ, Stone HL, Brown AM. Effects of unilateral stellate ganglion blockade on the arrhythmias associated with coronary occlusion. American Heart Journal. 1976;92(5):589-599. doi:10.1016/s0002-8703(76)80078-6.
- Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Executive summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society [published correction appears in Heart Rhythm. 2018 Sep 26;:]. Heart Rhythm. 2018;15(10):e190-e252. doi:10.1016/j.hrthm.2017.10.035
- Serna-Gutierrez J. Ultrasound-guided stellate ganglion block. Colombian Journal of Anestesiology. 2015;43(4):278-282.
- Kapral S, Krafft P, Gosch M, Fleischmann D, Weinstabl C. Ultrasound imaging for stellate ganglion block: direct visualization of puncture site and local anesthetic spread. A pilot study. Reg Anesth. 1995;20(4):323-328.
- Brown PK, Coffey WB. Surgical Treatment of angina Pectoris: Report of Eight Additional Cases and Review of Literature. Arch Intern Med (Chic). 1924;34(4):417–445.