The eye is a critical organ in our everyday life. We use the eye to help us navigate the world, communicate with others, and protect us from danger.
From 2005 to 2011, an estimated 11.9 million emergency department visits were for eye complaints (emergent and non-emergent).1 Urgent identification of vision threatening causes of eye emergencies is critical to saving a person's vision.
Eye emergencies can be due to traumatic or non-traumatic etiologies such as chemical burns, acute angle glaucoma, vascular compromise such as retinal artery/vein occlusion, or orbital compartment syndrome (OCS). Orbital varices, though rare, can cause orbital compartment syndrome leading to a vision-threatening emergency. It is important for an emergency physician to be able to recognize the signs and symptoms of orbital compartment syndrome and treat it urgently.
Case Presentation
A 39-year-old healthy woman presented to the emergency department with left eye swelling and pain worsening over 24 hours, vertical diplopia, headache, and vomiting. Physical examination was significant for right eye visual acuity of 20/25; left 20/30. Pupils were equal, round and reactive bilaterally with no afferent pupillary defect. Right intraocular pressure was 12 mmHg; left 11 mmHg.
Externally, there was 5 mm of relative proptosis and 4 mm of hyperglobus on the left. Full extraocular motility was intact bilaterally but painful with movements on the left. The patient had a remote history 18 years ago of her left eye bulging due to a "leaky blood vessel" but otherwise had no significant past medical history.
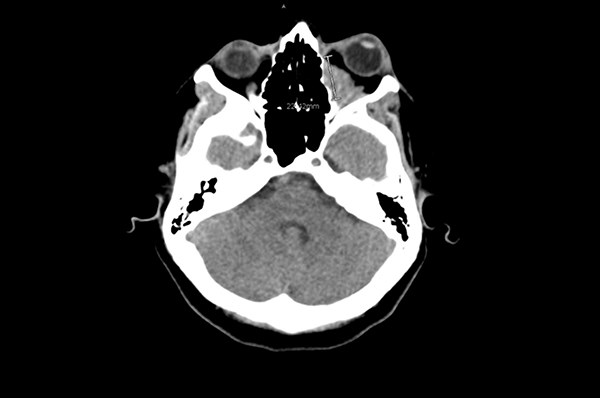
Computed tomography (CT) imaging was obtained, and ophthalmology was consulted. The patient was admitted for pain control, antiemetics, and systemic steroid therapy to reduce the associated edema. MRI was also obtained, demonstrating a heterogeneous, poorly circumscribed mass with variable areas of enhancement consistent with an orbital varix with acute hemorrhage. The patient did well and was discharged after 24 hours on long-term oral steroids without surgical intervention.
Discussion
Orbital varices represent less than 1.3% of orbital tumors.2 Malformations typically comprise single or multiple venous channels. Primary varices are congenital; secondary varices are arteriovenous malformations, carotid-cavernous fistulas, or dural arteriovenous fistulas that drain into the orbit.2,3 Orbital varices can cause ocular hemorrhage, thrombosis and optic nerve compression, causing pain, proptosis and visual changes.4 Diagnosis is by CT, MRI or ultrasound. Importantly, acute hemorrhage can result in sudden, increased intraorbital pressure resulting in OCS.
Orbital signs concerning for OCS include marked decreased visual acuity, afferent pupillary defect, proptosis, diffuse subconjunctival hemorrhage, chemosis, and pain with eye movement.
If signs of OCS are present, lateral canthotomy and inferior cantholysis are indicated to decompress the eye and preserve the patient's vision.5 Other key steps to managing these patients while in the emergency department include head-of-bed elevation of at least 45
degrees, pain control, antiemetic therapy, cough suppressants, antihypertensives, correction of any coagulopathy and reversal of anticoagulants if benefits outweigh risks. Some patients may require surgical intervention if they have nonresolving thrombotic episodes, disfiguring proptosis, or optic nerve compression.
References
1. Channa R, Zafar SN, Canner JK, Haring RS, Schneider EB, Friedman DS. Epidemiology of Eye-Related Emergency Department Visits. JAMA Ophthalmol. 2016;134(3):312-319.
2. Hacking C, Gaillard F. Orbital venous varix. Radiopaedia.org. Accessed 10/1/2017.
3. Midyett FA, Mukherji SK. Orbital Venous Varix. In: Midyett FA, Mukherji SK, eds. Orbital Imaging. Philadelphia, PA: Elsevier/Saunders; 2015:139–142.
4. Clemons KD, Burkat CN, Scawn R. Orbital varices. American Academy of Ophthalmology’s EyeWiki. Accessed 10/1/2017.
5. Gardiner MF. Overview of eye injuries in the emergency department. Torrey SB, Trobe J, eds. Waltham, MA: UpToDate Inc. Accessed 10/1/2017.