The most prevalent medical problems around the globe are in the sphere of headache disorders.
Between 50% and 75% of adults between ages 18-65 will have headaches. Worldwide, the disability and loss of productivity due to headache disorders is ranked third in the number of years lost to disability.1 However, primary headache disorders, of which migraines are the most prevalent, only account for up to 4% of chief complaints for emergency department (ED) admissions.1,2 Migraine therapies revolve around preventive measures in anticipation of migraines and adjuvant treatments for associated symptoms of migraines such as nausea and emesis. Another key therapy for migraines is abortive treatment. Preventative treatments include antidepressants, antihypertensive, ant antiseizure medications. However, triptans and NSAIDs are the mainstay of abortive treatment, which must be delivered at the onset of symptoms.1 This article intends to discuss the procedure, use, and relevance of Sphenopalatine Ganglion (SPG) blockade in the abortive treatment of migraines and other noteworthy primary headaches not due to trauma. The research behind SPG blocks and the application to ED use will also be discussed.
Research Behind SPG Blocks
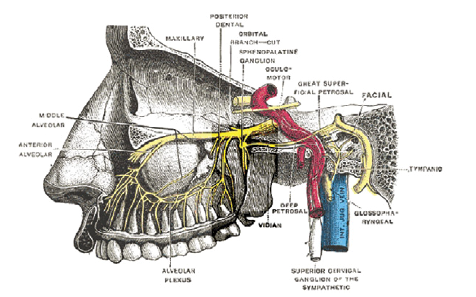
The culprit behind headache disorders are largely the nerves that converge at the sphenopalatine ganglion (SPG), an extracranial parasympathetic ganglion.3 The SPG is located behind the nasal bony structures, giving rise to the superior, inferior and posterior lateral nasal branches, nasopalatine nerve, greater and lesser palatine nerves, the pharyngeal branch of the maxillary nerve, and orbital branches that innervate the lacrimal gland.3,4 During a headache meninges become inflamed, leading to activated pain receptors per the trigeminal nerve. These pain receptors transmit impulses through the SPG to autonomic nerves.
SPG involvement results in lacrimation and nasal discharge noted in migraines and other primary headaches. In the midst of a migraine, parasympathetic outflow from the SPG results in cranial vasodilation. Inflammatory mediators are able to activate meningeal pain receptors leading to migraine pain.3
The SPG relays sensory, sympathetic, and parasympathetic pathways.4,5 Sensory pathways for pterygopalatine branches with the maxillary nerve to terminate at the trigeminal ganglion, innervating parts of the head and neck. Sympathetic pathways arise from the superior cervical ganglion to converge at the SPG to innervate vasoconstriction in the nasal cavity, upper pharynx and palate. The parasympathetic pathways arise from the superior salivatory nucleus to join the SPG, innervating the lacrimal, nasal, and other oropharyngeal glands.4,5 As such, blockade at the SPG theoretically should propagate relief of symptoms associated with a headache state: meningeal vessel inflammation, lacrimation, rhinorrhea.
SPG blocks have been shown to be effective in the reduction of headaches, including but not limited to cluster headaches, chronic migraine, refractory trigeminal neuralgia, and post-operative analgesia for endoscopic sinus surgery.5 Approaches within the studies considered in the literature do not all use the procedures noted in the SPG Procedures and Steps section of this article. Variable approaches included intranasal, intraoral, transcutaneous as well as the use of radiologically guided needles to achieve the desired a SPG block.5
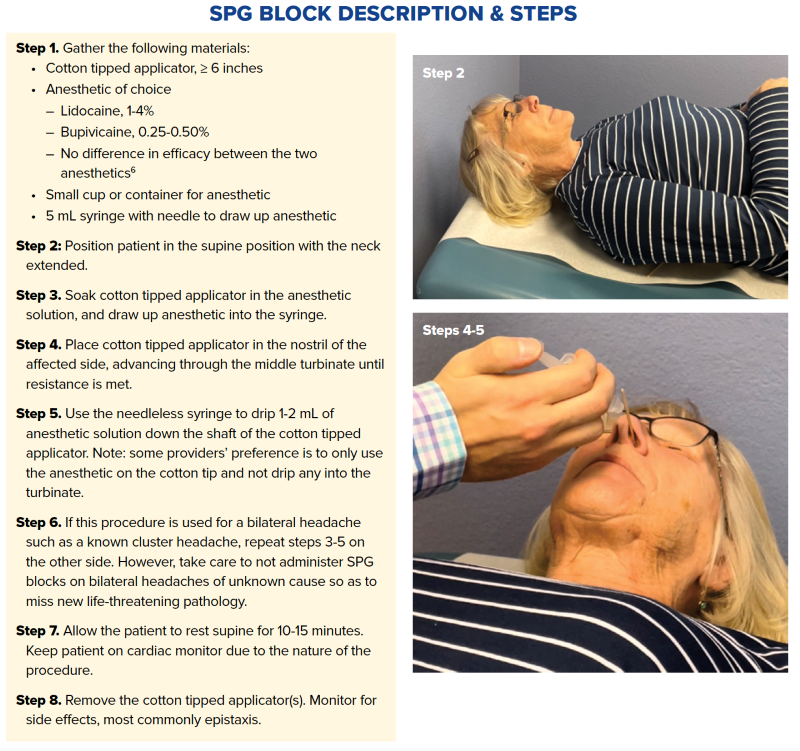
Immediately following the procedure, the patient may already be feeling relief! If they have numbness in the posterior pharynx, advise them not to eat or drink until full feeling returns.
Note: There are several proprietary applicators for blocking the SPG, with the SphenoCath® being the most studied. It can still be performed with an inexpensive simple cotton tip applicator but studies will need to be performed to determine any difference in efficacy.
Verdict: Is this realistic for use in EM?
Research behind SPG blocks is consistent in demonstrating efficacy in reducing or even resolving migraine headaches. It should be noted that many of the studies supporting SPG blocks are based in outpatient settings such as pain clinics. Anecdotally, these blocks’ efficacy can be externalized to the EM setting, but more research will need to be done to prove this.
Even if you are sold on the SPG block as an effective treatment for migraine headaches, it will not likely be your first approach to every patient with a migraine. Ordering prochlorperazine and diphenhydramine will remain an effective and relatively easy treatment for most migraines, and the medications take less time to order than it does to perform the SPG block procedure.
One strength of the SPG block, however, is that it has been shown to work relatively quickly. As much as 70% of migraines improved after 15 minutes in one case series, although bilateral blocks were utilized in this study.7 Other treatment remedies may have similar times to treatment success but would be more sedating and could require longer ED stays. Besides the time involved in the procedure, another downside of the SPG block is proposing to a patient that a cotton tip applicator be placed several inches into their nostril. However, given how prevalent placing nasal swabs in nostrils has become over the past year, this just may be time for the SPG block to shine.
Note: SPG anatomy image obtained from Wikimedia Commons; picture is public domain. All other images were taken with a volunteer in a non-clinical setting.
References
- Hovaguimian A. Headache and Facial Pain. In: Drislane FW, ed. Blue Prints Neurology, 5e. Wolters Kluwer Health, Inc 2019. 78-90
- Handschin N, Oppliger M, Brehm A, et al. Nontraumatic Headache in Adult Emergency Patients: Prevalence, Etiologies, and Radiological Findings. J Clin Med. 2020;9(8):2621. Published 2020 Aug 12. doi:10.3390/jcm9082621
- Viguri A, Paez Perez Y. Migraine Care: Why and How to Block the Sphenopalatine Ganglion Nerve. ACEPNow. 2018. https://www.acepnow.com/article/migraine-care-why-and-how-to-block-the-sphenopalatine-ganglion-nerve/ (accessed 5 Feb 2021).
- Ho KWD, Przkora R, Kumar S. Sphenopalatine ganglion: block, radiofrequency ablation and neurostimulation - a systematic review. J Headache Pain. 2017;18(1):118. Published 2017 Dec 28. doi:10.1186/s10194-017-0826-y
- Tolba R, Weiss AL, Denis DJ. Sphenopalatine Ganglion Block and Radiofrequency Ablation: Technical Notes and Efficacy. Ochsner J. 2019.19(1):32-37. doi:10.31486/toj.18.0163
- Kirkpatrick DL, Townsend T, Walter C. et al. Lidocaine Versus Bupivacaine in the Treatment of Headache with Intranasal Sphenopalatine Nerve Block. Pain Physician. 2020;23(4):423-428. PMID: 32709177.
- Binfalah M, Alghawi E, Shosha E, Alhilly A, Bakhiet M. Sphenopalatine Ganglion Block for the Treatment of Acute Migraine Headache. Pain Res Treat. 2018;2018:2516953. Published 2018 May 7. doi:10.1155/2018/2516953