Meredith Hill-Ciesielski, MD, Ultrasound Fellow, Detroit Receiving and Sinai Grace Hospital, Wayne State University, Detroit, MI
Mark Favot, MD, Director of Emergency Ultrasound, Sinai-Grace Hospital/DMC, Detroit, MI
Case
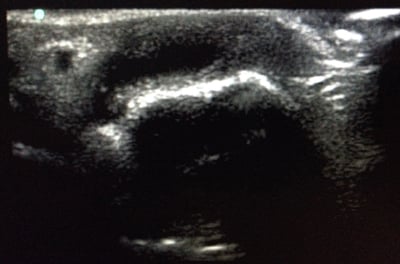
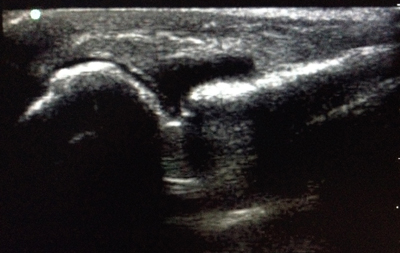
A 52-year-old male was diagnosed with gout three weeks ago, and is now complaining of two days of worsening pain in his hands and feet. He has been taking colchicine without any relief of his symptoms. Pain and swelling persist, and are particularly worse in his right hand. He has no history of IV drug use and has avoided alcohol and red meat. He is febrile to 38.6 °C, and an examination of the upper extremities reveals edema of the second and third metacarpophalangeal (MCP) joints of the right hand. The affected joints are tender and warm, with severely limited passive range of motion. A focused ultrasound of the right second MCP joint demonstrates a significant effusion (Images 1 and 2). Using ultrasound guidance, the joint is aspirated and returns approximately 2 ml of cloudy fluid that is sent for analysis. The joint aspirate shows 111,500 nucleated cells, and the patient is started on IV antibiotics and admitted after a hand surgery consult.
Discussion
Musculoskeletal ultrasound is a common diagnostic procedure in sports medicine and is becoming more common in emergency medicine. It has been used to aid in diagnosis and in arthrocentesis of larger joints such as the knee; however, it can be useful in the evaluation of all joints. Ultrasound can identify an effusion without the risk of radiation, which is of particular concern for pediatric and pregnant patients. It can also help to narrow the differential diagnosis when a patient's history and physical are equivocal, and can be particularly useful in cases where it is unclear based on clinical exam if the patient has skin cellulitis overlying a joint or septic arthritis. If ultrasound of the joint in question reveals no effusion, then septic arthritis has been essentially ruled out.
One study revealed that ultrasound might reduce unnecessary arthrocenteses in the ED. Fifty-four cases of potential septic arthritis were identified, and emergency physicians were asked to decide if an arthrocentesis should be performed based on physical exam of the joint alone. The study included a range of joints, 72% of which were planned for arthrocentesis as per the physician exam. Ultrasound performed on these joints reduced the number of ultrasounds performed to 37% of the total, based on presence or absence of an effusion.2 Joint ultrasound saved these patients from an invasive procedure and allowed the physician to better delineate between a soft tissue infection and possible septic arthritis. It is important to remember that the ability to detect an effusion with ultrasound is operator-dependent. There are currently no known clinical criteria capable of ruling out septic arthritis.3 Physical exam, history, and serum biomarkers used in the acute setting have not shown to significantly increase the post-test probability of septic arthritis.4 The use of ultrasound to identify a joint effusion can help emergency clinicians to risk-stratify their patients with suspected septic joints.
Ultrasound can be especially helpful in small joints where physical exam may fail to demonstrate a palpable effusion despite the presence of a relatively significant joint effusion. Assessing for effusion with ultrasound is more reproducible and accurate than physical exam alone.5 Once an effusion is identified, ultrasound can increase the success rate of arthrocentesis and can decrease the discomfort for the patient. When ultrasound guidance is utilized for arthrocentesis of the knee, patients report less pain and providers feel the exam is easier to perform.6 In a study comparing palpation and landmark-guided small joint arthrocentesis to ultrasound-guided arthrocentesis, those in the ultrasound-guided group had a success rate of 96%, compared to 59% in the palpation-guided group.7 It may be difficult or nearly impossible for the emergency physician to perform an arthrocentesis of smaller joints without ultrasound. The morbidity of undiagnosed septic arthritis, particularly in joints of the hand, is very high. Thus, it is imperative that emergency physicians become comfortable with using ultrasound for detection of joint effusion, especially in smaller joints.
The Procedure
To perform ultrasound-guided small joint aspiration, the joint is first evaluated in long axis using the high frequency linear array transducer. The probe should be positioned with the indicator pointing proximally. It is easiest to begin scanning over the proximal phalanx to identify the echogenic extensor tendon overlying the hyperechoic bone. Tendons are more echogenic than muscle, and will appear as parallel lines connecting bones to muscle.
Follow the proximal phalanx and extensor tendon proximally to the MCP joint (Image 3). By rotating the probe 90 degrees to the left, the short axis is visualized (Image 4). The anechoic synovial fluid will appear black on the ultrasound screen, whereas bone will appear hyperechoic and white. The joint space will be identified as a small anechoic space between the proximal end of the proximal phalanx and the distal end of the metacarpal. A septic joint will often have a hypoechoic appearance, with dependent internal echoes due to the purulence of the fluid in the joint. In image 2, there is a collection of fluid noted in the second MCP joint extending distally beneath the extensor tendon, which demonstrates a joint effusion.
Once the joint effusion is recognized on ultrasound, an ultrasound-guided arthrocentesis can be performed. There are no absolute contraindications to the procedure. All contraindications, including overlying cellulitis, are relative.1 Position the patient with his or her hand resting comfortably in a palm-side down position. The hand should be draped in sterile towels; the procedure is usually best performed with a Mayo stand.
Begin by thoroughly cleansing the skin. Lidocaine can be used for local anesthesia at the site of needle insertion; alternatively, a digital block may be used if necessary. The MCP joint should be imaged in the long axis using a linear array transducer with sterile probe cover. The probe indicator should be pointed proximally. Once the joint space is identified, it should be centered on the ultrasound screen. Because the MCP joint is so superficial, a medial or lateral out-of-plane technique is the preferred method for needle insertion.
Next, insert a 21-gauge needle attached to a 3-mL syringe in the dorsomedial or dorsolateral aspect of the joint toward the ultrasound probe, and under the extensor tendon (Image 5). Continuous negative pressure should be applied to the syringe plunger while advancing the needle. Advance the needle until the tip becomes visible underneath the tendon and inside the joint space on the ultrasound screen. Since the MCP joint is so small, only a few milliliters of fluid will be aspirated, even when the joint effusion is significant.