Brian C. Phillips, MD, Resident Physician, Emergency Medicine/Pediatrics, Indiana University, Indianapolis, IN
As few as 10-200 organisms may be sufficient to develop an infection
Case presentation
Your next patient is a 6-year-old girl with abdominal pain and diarrhea. Her mother tells you her daughter has had a fever, abdominal pain, and frequent bouts of watery, mucus-like diarrhea, and that today she saw blood in her stool. She has been eating and drinking well, and has had no vomiting or urinary complaints. She is otherwise healthy, and her immunizations are up-to-date. There has been no recent travel, but she does attend daycare while her parents are at work. On examination, her temperature is 100.9F, HR 116, BP 102/55, RR 20, and SpO2 100%. She appears to be well-hydrated. Her abdomen is diffusely tender to palpation, but without peritoneal signs. Her mother is concerned because she heard something on the news about an outbreak of potentially life-threatening bacterial diarrhea, and so she is requesting antibiotics.
What's in the bloody differential?
Parents are often concerned about the color of their child's stool – especially if there is the appearance of blood. Many foods can mimic hematochezia after their transit through the GI tract. If clinical suspicion is low, a hemoccult test can often help the clinician and alleviate parents' fears, though false positives can occur. If blood is present, the differential diagnosis in the pediatric population is vast. More serious causes of GI bleed in the child include intussusception, a Meckel's diverticulum, necrotizing enterocolitis, inflammatory bowel disease, and toxic ingestion. Bacterial dysentery (e.g., diarrhea with blood and mucus) should be considered, especially if symptoms include fever, greater than 10 stools in 24 hours, or travel outside of the U.S.1 Of infectious diarrheal cases, bacteria have been implicated in up to 20%.2 Other historical features that are positively associated with bacterial pathogens include abdominal tenderness, duration <10 days, symptom onset between the months of May and October, and lack of vomiting.1,3 Parents may request antibiotics, so knowledge of historical differences between bacterial and viral etiologies of diarrhea can help with antibiotic stewardship. When the diagnosis suggests a bacterial etiology, the most common culprits are Escherichia coli, Shigella, Salmonella, and Campylobacter species.
Working out the workup
If a bacterial pathogen is considered likely, a sample of the stool should be sent for culture. Although not a sensitive test, the results can be very important with regard to public health surveillance. In a well-appearing child with diarrhea, further workup is not necessary. If there is concern for an electrolyte imbalance or hemolytic uremic syndrome (HUS), additional lab work may be indicated. Fecal leukocyte testing is neither sensitive nor specific enough to change management decisions.2 Examination for ova and parasites may be indicated in immunosuppressed patients, those with chronic diarrhea, or after known/possible exposure (travel to developing countries, known outbreaks).2 Clostridium difficile toxin assay is recommended only in the appropriate clinical context.4 It is important to remember that as many as 40% of children < 1 year old may be colonized and therefore test positive for the toxin (after age 3, carriage rates approximate those in adults).4
Most cases of acute bacterial enteritis resolve without antibiotic therapy. In fact, there is some debate whether antibiotic therapy for dysentery increases the risk of developing HUS – especially in those infected with Shiga toxin-producing E. coli O157:H7.5 However, a meta-analysis of the available research failed to demonstrate that antibiotics increase the risk of HUS.6 The risk of developing HUS in non-Shiga toxin-producing bacterial infections is very low.
Shigella outbreak?
The patient's mother was referring to the increase in cases of shigellosis reported in central Indiana, where her daughter had been attending daycare. In the U.S. there have been many epidemics of shigellosis reported in the literature, especially in daycare settings. There are four common serotypes of Shigella: S. sonnei, S. flexneri, S. boydii, and S. dysenteriae. In 2012 the CDC reported that 75% of the isolates were of the subtype S. sonnei.7 Only 0.3% of the Shigella isolates were of the subtype S. dysenteriae, which is known to produce Shiga toxin (the others do not). This subtype causes more severe disease, and has a greater association with HUS.8
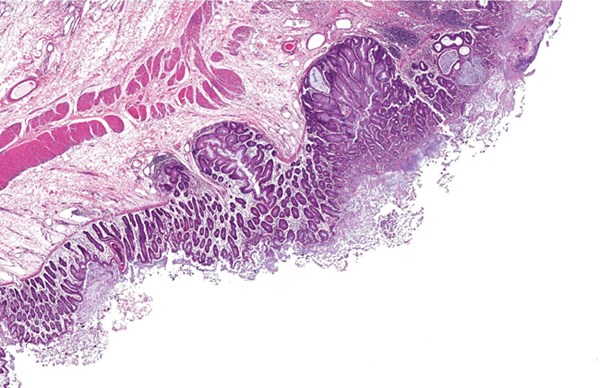
Shigella species are transmitted via the fecal-oral route and can contaminate inanimate objects, food, and water. Depending on the patient scenario, ingestion of as few as 10-200 organisms may be sufficient to develop an infection. The incubation period is 1 to 3 days (range 1 to 7 days). The symptoms range from watery stools to acute dysentery, with many suffering from fevers, abdominal pain, and mucoid or bloody stools. The classically taught complication of generalized seizure is not common, and its pathophysiology is not well understood. Other potential consequences of Shigella infection include toxic megacolon, sepsis, and HUS.
Despite the potentially serious complications, most cases of S. sonnei shigellosis are mild and symptoms typically resolve in 2 to 3 days, making it a self-limited disease. However, the carrier state can be prolonged, lasting as many as 4 weeks. Antibiotics can help reduce the duration of symptoms and decrease the length of the carrier state. It may be important from a socioeconomic standpoint to start treatment early; for each day that the child must remain out of daycare (or school), the parent must arrange an alternative form of childcare or take off from work.
The majority of S. sonnei isolates are now resistant to trimethoprim/sulfamethoxazole and ampicillin. Current therapies for children include azithromycin as a first-line agent8 (12mg/kg up to 500 mg on the first day, and 6mg/kg up to 250mg on days 2 through 5), cefixime, parenteral ceftriaxone, or a fluoroquinolone (not approved for patients <18, though they have been used successfully).9 The first-line therapy for adults is a fluoroquinolone, typically ciprofloxacin.
What do I tell Mom?
As with most problems, return precautions and follow-up instructions are crucial, especially in the pediatric population. It is also important to check your local health department recommendations during any epidemic. All four of the most common bacterial enteritis-causing organisms are reportable to the health department. More information can be found on local health department and CDC websites. You should know the guidelines so that you can provide the appropriate instruction to parents. For instance, the Marion County Public Health Department in Indiana requires that infected children be excluded from daycare until they have COMPLETED antimicrobial therapy (OR have two successive negative stool cultures), AND have been symptom-free for >24 hours. The rules for healthcare or daycare workers and food handlers are even stricter: they must be asymptomatic for >24 hours AND have TWO successive negative stool cultures (collected 24 hours apart). There is no need to treat asymptomatic contacts prophylactically.
Case resolution
While stool culture results were pending, our patient was treated with a 5-day course of azithromycin with the presumptive diagnosis of shigellosis. During this outbreak, the pre-test probability of Shigella was sufficiently high to further support early empiric therapy. The patient did well and returned to daycare after resolution of her diarrhea and completion of the 5-day course of antibiotics. Three days after her visit to the ED, her stool culture results were finalized: Shiga toxin-negative, Shigella sonnei, resistant to trimethoprim/sulfamethoxazole.
References
- Klein EJ, Boster DR, Stapp JR, et al: Diarrhea etiology in a children's hospital emergency department: a prospective cohort study. Clin Infect Dis 43:807-813, 2006.
- Chen, Lei: ”œInfectious diarrheal disease and dehydration,” in Rosen's Emergency Medicine 7th ed, Vol 2, edited by Marx, Hockberger, Walls et al, p 2188, Elsevier, Philadelphia, 2010.
- Finkelstein JA, Schwartz JS, Torrey S, et al: Common clinical features as predictors of bacterial diarrhea in infants. Am J Emerg Med 7:469-473, 1989.
- Schutze GE, Willoughby RE: Clostridium difficile infection in infants and children. Pediatrics 131(1):196-200, 2014.
- Wong CS, Jelacic S, Habeeb RL, et al: The risk of the hemolytic-uremic syndrome after antibiotic treatment of Escherichia coli O157:H7 infections. NEJM 342(26):1930-1936, 2000.
- Safdar N, Said A, Gangnon RE, et al. Risk of hemolytic uremic syndrome after antibiotic treatment of Escherichia coli O157:H7 enteritis: A meta-analysis. JAMA 288(8):996-1001, 2002.
- Centers for Disease Control and Prevention (CDC). National Shigella surveillance annual report, 2012. Atlanta, Georgia: US Department of Health and Human Services, CDC, 2014.
- Pickering LK, Dimberlin DW, Long SS: ”Shigella Infections,” in Red Book: Report of the Committee on Infectious Diseases, 29th ed, edited by LK Pickering, p645, Elk Grove Village, American Academy of Pediatrics, Chicago, 2012.
- Velissariou, I.M., The use of fluoroquinolones in children: recent advances. Expert Rev Anti Infect Ther, 2006. 4(5): p. 853-60.