What EM Residents Need to Know
Sepsis definitions were last revised in 2001. Since then, discoveries have been made regarding the pathobiology, management, and epidemiology of sepsis. In 2014, the Society of Critical Care Medicine and the European Society of Intensive Care convened a task force to produce the Third International Consensus Definitions for Sepsis and Septic Shock.1 Existing sepsis definitions were felt to place excessive focus on inflammation, and systemic inflammatory response syndrome (SIRS) criteria were found to have inadequate sensitivity and specificity for sepsis. Furthermore, unclear definitions of organ dysfunction and septic shock were felt to contribute to large differences in sepsis incidence and mortality across epidemiological studies.
Methods
To inform their decisions, the task force first conducted a systematic review and meta-analysis of previously published epidemiological studies and cohort studies using the Surviving Sepsis Campaign registry and electronic health record (EHR) data sets.2,3 Using this data, the task force used a Delphi process to reach a consensus.2 A Delphi process is a systematic and interactive forecasting method in which a series of surveys are conducted by a panel with the goal of reaching a convergent opinion. New criteria were defined and validated in separate EHR data sets.3
Multivariable logistic regression was used to identify a new clinical model, termed quick SOFA (qSOFA), in which any 2 of 3 clinical variables—Glasgow Coma Scale score less than 15, systolic blood pressure of 100 mm Hg or less, and respiratory rate 22/min or greater—offered similar predictive validity to that of the full Sequential Organ Failure Assessment (SOFA) score outside of the ICU (Table 1).1
New Recommendations
Updated definitions, clinical criteria, and associated mortality are provided in Table 2. The task force utilized the previously described SOFA score as part of the clinical criteria for sepsis (Table 3).4 The SOFA score is an existing scoring system for organ dysfunction well known within the critical care community. High SOFA scores are associated with an increased probability of mortality, with a mortality rate of 9% for ICU patients with no organ failure on admission, and increasing to 82.6% for ICU patients with four or more failing organs.5 The idea behind the novel qSOFA score is to provide quick bedside criteria to help identify adult patients with suspected infection in out-of-hospital, emergency department, and ward settings who are likely to have poor outcomes.
Clinical Impact
The authors concluded that the updated definitions will provide greater consistency for future research and facilitate timely detection and treatment of patients with sepsis or those at risk of developing sepsis.
qSOFA has the potential to be used as the new sepsis screening tool in pre-hospital, emergency department, and inpatient settings. In patients with known or suspected infection, it could replace SIRS as a new tool used to trigger sepsis alerts which have been targeted in hospitals' efforts to meet federal quality standards.
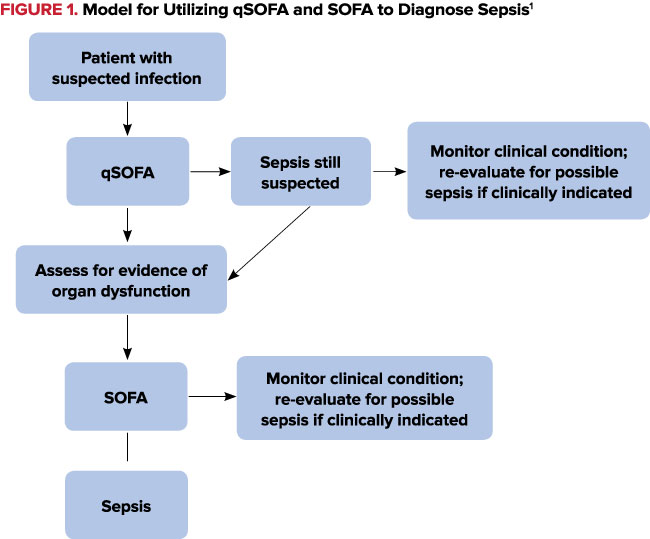
How to Use qSOFA and SOFA
It is important to remember that qSOFA was developed as a risk stratifier, not as a screening tool. However, given that the new definition of sepsis implies increased mortality, after suspecting or identifying infection, qSOFA can then be used as a screening tool for sepsis. Clinicians must still use their clinical gestalt first to decide if an undifferentiated patient could have an infection. Only then is it appropriate to apply qSOFA.
Even if a patient with a presumed infection does not meet qSOFA criteria, if sepsis is still suspected, clinicians should proceed to assess for evidence of organ dysfunction utilizing the SOFA score (Figure 1). A patient with a SOFA score ‰¥2 can then be diagnosed with sepsis.
Finally, if a septic patient is requiring vasopressors to maintain a MAP ‰¥65 mm Hg and has a persistent lactate >2 mmol/L (18 mg/dL) despite adequate fluid resuscitation, this patient is in septic shock.
FAQs
Q. How do I score SOFA in my patients with chronic organ dysfunction, such as those with end-stage renal and end-stage liver disease who have baseline lab abnormalities?
A: These patients have worsening organ dysfunction if their SOFA score is ‰¥2 points higher than their baseline labs.
Q. What is adequate fluid resuscitation?
A: No consensus exists. Previous sepsis guidelines have recommended fluid resuscitation with a minimum of 30 ml/kg crystalloid bolus within the first three hours of management.8 Within Sepsis-3, criteria for adequate fluid resuscitation were not defined because this variable is highly user dependent. However, the authors described that if a patient's hypotension is fluid responsive (presumably with any amount of fluids), thus not requiring the use vasopressors, this patient does not meet criteria for septic shock.
Table 1. qSOFA (Quick Sofa) Criteria1
| Altered mentation (GCS <15) |
| Systolic blood pressure <100 mm Hg |
| Respiratory rate >22/min |
Table 2. New Sepsis and Septic Shock Definitions, Criteria and Associated Mortality
| Previous definition | Sepsis-3 definition | Clinical criteria | Associated mortality | |
| Sepsis | 2 or more SIRS criteria in the setting of infection6,7 | Life-threatening organ dysfunction caused by a dysregulated host response to infection1* | Suspected or documented infection and an acute increase of ‰¥2 SOFA points (a proxy for organ dysfunction)1 | A SOFA score ‰¥2 reflects an overall mortality risk of approximately 10% in a general hospital population with suspected infection1 |
| Septic Shock | Sepsis with arterial hypotension despite adequate fluid resuscitation (30 ml/kg fluid bolus)6,7 | A subset of sepsis in which underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality1 | Sepsis and vasopressor therapy needed to elevate MAP ‰¥65 mm Hg and actate >2 mmol/L (18 mg/dL) despite adequate fluid resuscitation1 | Hospital mortality is in excess of 40%1 |
*Replaces severe sepsis, previously defined as “sepsis complicated by organ dysfunction.”7
Table 3. Sequential Organ Failure Assessment (SOFA) Scorea
| System | Score 0 | 1 | 2 | 3 | 4 |
| Respiration PaO2/FiO2, mm Hg |
‰¥400 | 400 | 300 | 200 | 100 |
| Coagulation Platelets, x103/μL |
‰¥50 | 150 | 100 | 50 | 20 |
| Liver Bilirubin, mg/dL |
1.2 | 1.2”“1.9 | 2.0”“5.9 | 6.0”“11.9 | 12 |
| Cardiovascular mm Hg, μg/kg/min for at least 1 hour |
MAP ‰¥70 | MAP 70 | Dopamine 5 or any dose of dobutamineb |
Dopamine 5.1-15 or epinephrine ‰¤ 0.1 or norepinephrine ‰¤0.1b | Dopamine 15 or epinephrine 0.1 or norepinephrine 0.1b |
| CNS Glasgow Coma Scale |
15 | 13”“14 | 10”“12 | 6”“9 | 6 |
| Renal Creatinine mg/dL or urine output mg/day |
1.2 | 1.2”“1.9 | 2.0”“3.4 | 3.5”“4.9
or <500 |
5.0
or <200 |
Abbreviations: FiO2, fraction of inspired oxygen; MAP, mean arterial pressure; PaO2, partial pressure of oxygen. a Adapted from Vincent et al. 4 b Catecholamine doses are given as μg/kg/min for at least 1 hour.
Limitations
Prospective studies are needed to gauge the impact of SOFA and qSOFA on morbidity and mortality and whether they lead to a change in management in practice.
Emergency medicine (EM) experts were not a part of the task force, and no EM organizations have endorsed the new definitions. Future consensus statements regarding the early identification and treatment of sepsis will need to include representation from EM physicians, who are among the clinicians most often diagnosing and initiating management of sepsis.
Take-Home Points
- Sepsis is now defined as life-threatening organ dysfunction (an acute increase of ‰¥2 SOFA points) caused by a dysregulated host response to infection.
- Septic shock is a subset of sepsis in which underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality. These patients require vasopressor therapy to elevate MAP ‰¥65 mm Hg and have a lactate >2 mmol/L (18 mg/dL) despite adequate fluid resuscitation.
- SOFA can be used to score organ dysfunction and predict hospital mortality in septic patients.
- qSOFA can be rapidly scored at the bedside and can facilitate prompt recognition of life-threatening infection and thus assist the EM physician in prioritizing resuscitative efforts and making triage decisions. See qsofa.org for more information and a qSOFA calculator.
References
- Singer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801-810.
- Shankar-Hari M, et al. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock. JAMA. 2016;315(8):775-787.
- Seymour CW, et al. Assessment of Clinical Criteria for Sepsis. JAMA. 2016;315(8):762-774.
- Vincent JL, et al. Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22(7):707-710.
- Vincent JL, et al. Working Group on “Sepsis Related Problems” of the European Society of Intensive Care Medicine. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Crit Care Med. 1998;26(11):1793-1800.
- Bone RC, et al. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med.1992;20(6):864-874.
- Levy MM, et al. International Sepsis Definitions Conference. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003;29(4):530-538.
- Dellinger RP, et al. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012. Intensive Care Med. 2013;39:165”“228.