Emergency medicine residency prepares physicians to deliver compassionate, evidence-based, and up-to-date patient care in the emergency department. An additional, essential, and fundamental topic worthy of intentional time and education is the physician reimbursement process. Just as the health care landscape evolves over time, so do the intricacies and nuances of how emergency care is reimbursed.
In January 2023, policymakers launched a once-in-a-generation comprehensive overhaul and monumental pivot to how our specialty gets reimbursed. They did this by completely modernizing our documentation guidelines.
This paper highlights three aspects of EM physician reimbursement:
- EM coding and documentation
- Physician payment and reimbursement
- Procedures and critical care
Section 1: EM Coding and Documentation
Documentation should serve to provide a complete account of the patient’s presentation and ED course in the emergency department. In addition to providing a documented history of the patient encounter, documentation is essential for billing purposes by assigning level codes to patient care and/or procedures. These codes assigned to billing are Current Procedural Terminology, or CPT, maintained by the American Medical Association (AMA) since 1966. This code set is updated annually by an advisory committee made up of representatives from each specialty society. CPT codes describe the cognitive and procedural work emergency physicians provide during patient care.
The International Classification of Diseases 10th Edition, or ICD-10, codes are used to communicate patient diagnoses to insurance companies. These codes are different from CPT coding and serve a different purpose. While ICD-10 codes provide diagnoses, CPT codes reflect work and cognition performed by the physician to arrive at that diagnosis. Unfortunately, some payers use the discharge ICD-10 codes to limit payment for certain discharge diagnoses; however, if the emergency physician also documents their differential diagnosis, interventions, and cognitive processes to arrive at the discharge or admitting diagnoses, the CPT code used to bill for the encounter should accurately reflect the work performed.
Enacted in 1999, The Prudent Layperson (PLP) Standard established the principle of reimbursing the work done to establish a medically emergent condition and the subsequent care and treatment for this patient, regardless of the final diagnosis. The Prudent Layperson language, adopted individually by most states, defines an emergency medical condition as a medical condition manifesting itself by acute symptoms of sufficient severity (including severe pain) such that a prudent layperson, who possesses an average knowledge of health and medicine, could reasonably expect the absence of immediate medical attention to result in: (a) placing the patient’s health in serious jeopardy; (b) serious impairment to bodily functions; or (c) serious dysfunction of any bodily organ or part. Downcoding charts based on discharge diagnoses that are less severe than others forces the patient to decide if they truly have an emergent condition or not. That is the role of the EM physician, and forcing a patient to do so is a clear PLP standard violation.
Earlier this year, significant modifications were made to the ED evaluation and management (E/M) code set (99281-99285), which now are solely determined by the Medical Decision Making (MDM) components of your documentation. Three components are used to determine the appropriate E/M code:
(1) Complexity of Problems Addressed (COPA)
(2) Data Reviewed and Analyzed
(3) Risk of Complications and Morbidity or Mortality
The highest two scores out of the three components determine the level of CPT coding.
To learn more about the 2023 E/M documentation changes, please refer to A Worthy Investment: What Every EM Resident Needs to Know About Reimbursement In 2023, published Feb. 22, 2023, on emresident.org.
Section 2: Physician Payment and Reimbursement
In U.S. payment models, physicians can receive reimbursement through productivity measures known as the Relative Value Unit, or RVU. An RVU is the universal metric of physician effort and the building block of payment. Each CPT E/M and procedure code is assigned a certain number of RVUs based on determinations from the Relative Value Scale Update Committee (RUC) composed of representatives from member specialties who provide recommendations to the Centers for Medicare and Medicaid Services (CMS) for the Medicare Physician Fee Schedule. ACEP holds the only permanent seat representing emergency medicine. Assigned RVU valuations reflect both the cognitive nature of patient care as well as the procedural work performed by the physician. (See Figure 1).
Figure 1
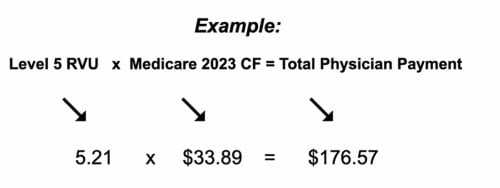
Total RVUs are calculated by taking the sum of physician work, practice expenses, and professional liability insurance. There also exists a Geographic Practice Cost Index (GPCI), where a cost differential exists based on practice location. Each RVU component is adjusted based on local cost index and multiplied by the Medicare Conversion Factor (CF) to determine final payment. It is important to note that RVUs increase with each increase in E/M CPT level. A formula can be used by emergency physicians to determine their productivity: RVU/Hour = RVU/Patient x Patients/hour. (See the Example Graphic and Table 2 below.)
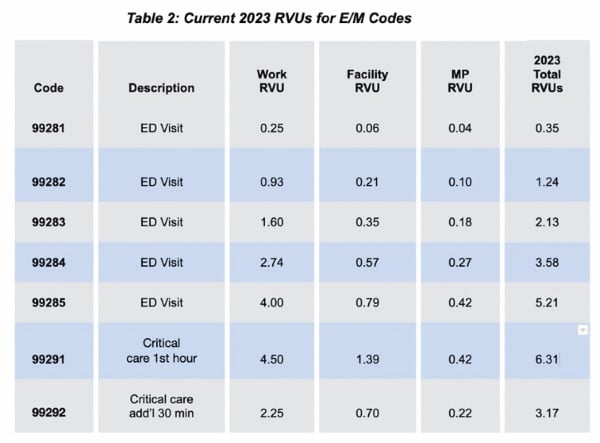
Note: MP = Liability insurance, Facility = practice expense)
Section 3: Procedures and Critical Care
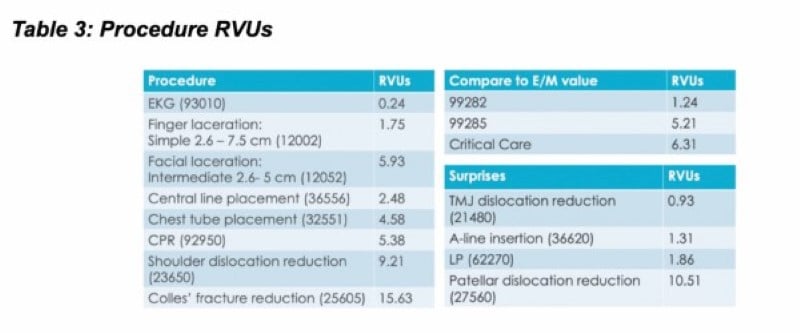
Most (90%) of the RVUs and reimbursement in EM come from the ED E/M codes 99281-99285. Procedures make up 9% of RVU-related reimbursement, while critical care performed by emergency physicians makes up 8% of the total RVU-related reimbursement. Table 3 demonstrates common procedures and RVUs that emergency physicians perform.
Critical care is defined as an illness or injury that acutely impairs one or more vital organ systems with probability of imminent or life-threatening deterioration expected in the patient’s condition. To bill for critical care, there must exist a suspicion that failure to initiate interventions on an urgent basis would lead to sudden, clinically significant, or life-threatening deterioration in the patient’s condition. Critical care must have documentation of at least 30 minutes of service spent directly managing the patient, resuscitating the patient, reviewing laboratories and imaging, or discussing the patient’s care with specialists or consultants. Critical care is the only time-based code in EM. Time spent on procedures such as CPR or intubation is separately billed and does not count toward critical care; it must be deducted from the time claimed as critical care.
Helpful 2023 Documentation Guideline Tips
Did you…
- Thoroughly and accurately document the chief complaint(s) and a detailed, complete MDM? The MDM is the most important factor in determining E/M level coding. It is essential to understand the documentation components that will allow the MDM coding to accurately reflect the work performed.
- Document abnormal vital signs and abnormal diagnostic test results?
- Record a medically appropriate history and physical exam?
- Document social determinants of health (i.e., housing, food, transportation insecurity, substance abuse, etc.) and how they have significantly impacted a patient’s care plan?
- Accurately document your procedure and/or sedation note? Learn what elements are required to generate a full and complete procedure note for commonly performed procedures (for example: site, size, technique, and complexity).
- Document your own interpretation of the ECG, monitor strip, and imaging (as your clinical skills afford)?
- Document any and all conversations with family, consultants, or specialists?
- Complete your charts in a timely manner?
Remember that documentation is not only used for billing, but for clinical care and medical-legal purposes as well. “Think in Ink” — If you did it, document it.
Conclusion
This is a limited summary to provide some introductory knowledge on how an emergency physician receives reimbursement for services and patient care provided. For further details and more information, make sure to read A Worthy Investment: What Every EM Resident Needs to Know About Reimbursement In 2023 on emresident.org.
Acknowledgements
Drs. Alexa Golden, Nicholas Cozzi, and Brian Hiestand are members of ACEP’s Reimbursement Leadership Development Program. Thank you to ACEP’s Reimbursement Committee as well ACEP’s Coding and Nomenclature Committee for expert consultation.



