Purple urine bag syndrome, first reported in 1978, is a subset of catheter-associated urinary tract infection.
Case
A male in his 70s with a past medical history of prostate cancer with metastases to his thoracic and lumbar spine presented to the emergency department with acute on chronic lower back pain. He underwent a laminectomy 3 weeks prior and has urinary outlet obstruction with bilateral nephrostomy tubes and an indwelling urinary catheter.
His physical exam is remarkable for tachycardia and baseline lower extremity deficits which include decreased sensation and motor function of the bilateral lower extremities. The differential diagnosis includes post-operative complications or infection from his recent laminectomy, pathologic fracture, epidural hematoma, catheter-associated urinary tract infection (CAUTI), nephrostomy tube dysfunction, and worsening structural back pain from his malignancy.
His laboratory workup was significant for leukocytosis of 15,000, C-reactive protein of 280, and a urinalysis (UA) showing large leukocyte esterase, 73 WBCs, and 507 RBCs. CT abdomen and pelvis with IV contrast showed properly functioning nephrostomy tubes without emergent or acutely significant findings. Given the patient’s recent intervention neurosurgery was consulted. There was low suspicion for post-op complication after their evaluation and further infectious work-up was recommended.
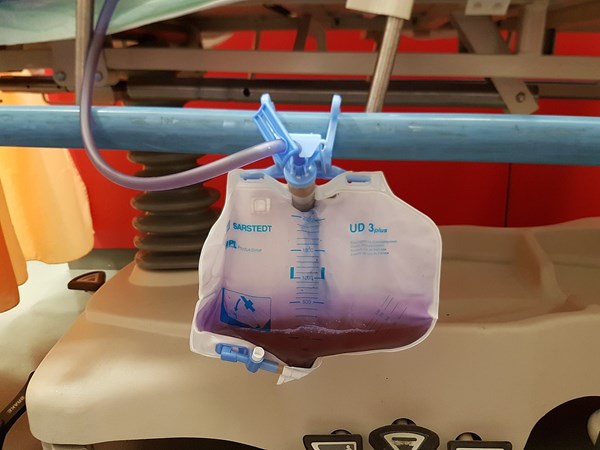
On re-examination his pain and tachycardia had improved with acetaminophen. Shortly thereafter the nurse drew our attention to a previously unrecognized bag of purple urine. This finding prompted several questions:
- What is the diagnosis?
- Does it represent CAUTI?
- What is the management strategy?

Discussion
This case demonstrates a rare condition known as Purple Urine Bag Syndrome (PUBS). An unmistakable visual, PUBS represents an uncommon side effect of urinary tract infections occurring most commonly in those with chronic indwelling urinary catheters.
Though not fully understood, the purple discoloration is believed to be created by a unique microbiologic and biochemical interplay. Metabolites of tryptophan get broken down by bacteria in the gastrointestinal (GI) tract and produce indoles. These compounds get absorbed in the blood and ultimately renally excreted. In the presence of an alkaline environment such as urine, bacterial flora commonly associated with colonization (ie, Klebsiella, Proteus, E. coli) produce sulphatases and phosphatases that convert the indoles to indigo (blue) and indirubin (red).
Risk factors for this phenomenon include those which increase bacteria in the GI tract (constipation) and urinary tract (female anatomy, elderly population, chronic catheterization).
Management
After clinching the diagnosis, the next step in management is to differentiate CAUTI from catheter-associated asymptomatic bacteriuria (CA-ASB). According to the most recent guidelines from the Infectious Disease Society of America, CA-ASB in patients with indwelling urethral catheterization is defined by the presence of ⩾105 cfu/mL of ⩾1 bacterial species in a patient without symptoms compatible with UTI, regardless of whether the urine is cloudy or malodorous. CA-ASB is typically managed conservatively and without antibiotics.
Alternatively, CAUTI is characterized by urinary symptoms and the presence of ⩾103 cfu/mL of ⩾1 bacterial species with no other identified source. As it pertains to our case, signs and symptoms of CAUTI in a patient with a spinal cord injury also include increased spasticity, back pain, autonomic dysreflexia, and/or sense of unease.
By definition PUBS is a subset of CAUTI. Treatment of CAUTI and PUBS are similar and typically include antibiotic therapy tailored to sensitivities derived from a urine culture. In the case of PUBS, the five most commonly cultured bacteria are E Coli, Enterococcus spp., Proteus spp., M. morganii, and Klebsiella spp. Since the majority of these bacteria are gram negative, ciprofloxacin is the most frequently cited antibiotic of choice. As an exception, fluoroquinolones are not recommended as a first-line therapy against enterococcus, and broader coverage should be provided initially. As a rule of thumb, best practice dictates antibiotic coverage guided by your hospital’s microbial resistance patterns and antibiogram.
Case Resolution
The patient's urine culture grew Enterococcus faecalis that was sensitive to and successfully treated with a course of fluoroquinolones.
PUBS FAST FACTS
- First reported in 1978
- Associated with women, chronic indwelling catheters, constipation, institutionalization
- Require treatment when patient experiencing symptoms of UTI
- Common bacterial causes: coli, Enterococcus spp., Proteus spp., M. morganii, and Klebsiella spp.
- Ciprofloxacin is a good choice if a culture is not yet available.
References
- Yang HW, Su YJ. Trends in the epidemiology of purple urine bag syndrome: a systematic review. Biomed Rep. 2018;8(3):249-256.
- Hooton MT, Bradley FS, Cardenas D, et al. Diagnosis, Prevention, and Treatment of Catheter-Associated Urinary Tract Infection in Adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(5):625-663.
- Yadav S, Rawal G, Singh A. Purple Urine Bag Syndrome: Are We Aware?. J Integr Nephrol Androl. 2016 [cited 2020 May 7]; 3:133-5. Available from http://www.journal-ina.com/text.asp?2016/3/4/133/193518
- Al Montasir A, Al Mustaque A. Purple urine bag syndrome. J Family Med Prim Care. 2013;2(1):104‐105.