At a time of year when most of us would prefer to be celebrating our incoming class of residents, instead EM-bound students, residents, and faculty have spent the past few months discussing the Match.

Questions cast uncertainty upon the future of our specialty. We have been asked about the numbers, the possible causes, if these trends will continue, and what will reverse these trends and strengthen our specialty.
EMRA cannot promise answers to all of these questions, but we have identified factors at play that point to potential solutions. And now, we’re sharing what we’ve learned so that you can be part of the response.
The Tipping Point
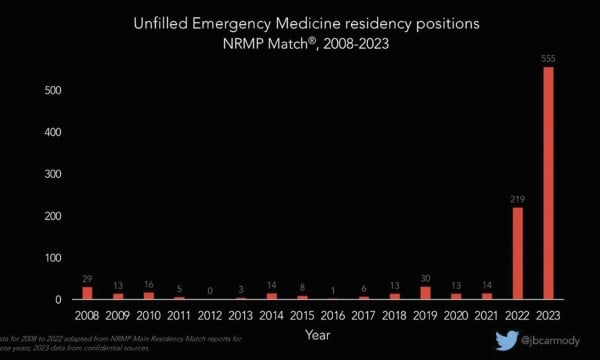
For years, applicants to EM have increased in parallel with the increase in residency positions. Consistently, there have been a greater number of applicants than residency positions. Unfilled spots were under 30 per year for more than 15 years.1
Applicants to EM peaked in 2021, coinciding with the initial surge of public support for frontline health care workers amid the COVID-19 pandemic. In the 2022 Match, applicants began to decrease, while spots continued to increase. This resulted in 219 unfilled emergency medicine residency positions through the 2022 Match, almost all filled in the Supplemental Offer and Acceptance Program (SOAP).2
In this year’s Match, applicants continued to decrease while spots continued to increase. Pre-SOAP, only 82% of EM positions were filled, the second-lowest match rate of all specialties. This resulted in 554 unfilled EM positions,2 of which a reported 501 have been filled after the SOAP (though official data is pending).
The supply-demand curve has shifted in ways that affect all of us in emergency medicine.
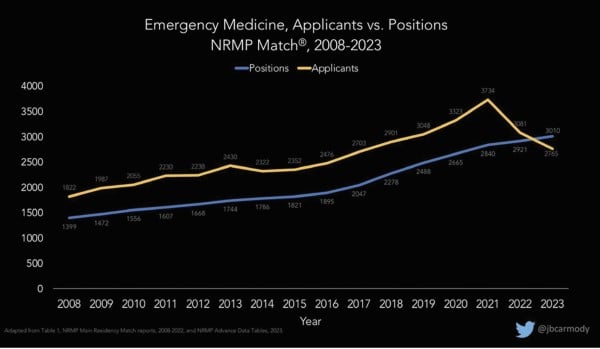
Graph courtesy of Bryan Carmody, DO. Used with permission.
Demand
The total number of applicants applying to EM has fallen by 17.5% since its peak in 2021 and now is approaching 2019 levels. Among MD applicants, the drop is even steeper. MD applicants fell from 2,385 at their peak two years ago to 1,460 — a 38.8% decrease. DO and IMG applicants also decreased, but to a lesser degree.
Historically, medical students have had more opportunities to experience EM and find mentorship. Some have speculated that recent classes missed those experiences due to the COVID-19 pandemic limiting in-person workshops and clinical experiences. However, a more concerning possibility is that students with more access to emergency departments may have seen the burnout, boarding, and other frustrations that make work more difficult for those in the ED. When EMRA called upon medical students to share their reasons for reconsidering a career in emergency medicine, a few cited discouraging experiences with some faculty and residents on shift.
Students also are concerned by gloomy predictions for the EM job market. The 2021 report “The Emergency Medicine Physician Workforce: Projections for 2030” forecasted a surplus of 7,845 EM physicians by 2030.3 EMRA’s medical student members reported that, for those saddled with hundreds of thousands of dollars in debt or committed to working in a specific region, the concern about saturated job markets was enough to drive them away. They also reported they had been cautioned by their deans and non-EM advisors not to pursue EM out of concern for workforce projections. In response to the workforce report, EMRA countered with an extensive analysis titled “Unity, Purpose, and Passion: Influencing the Future of the EM Workforce.”4
Supply
Meanwhile, residency positions have grown significantly during the past decade.
As a disclaimer, there are some new and established programs that are expanding sustainably. These programs have adequate leadership, clinical acuity, and procedural training to sustain a larger complement of residents, and residents graduate into communities that can support this growing pipeline of EM physicians.
However, there are also likely financial incentives for hospitals to open new programs or rapidly expand existing ones. In staffing emergency departments, residents earn lower salaries than attendings and most physician assistants and nurse practitioners, and part of resident salaries are government funded.
As such, for-profit hospital corporations like HCA have been implicated in the rapid expansion, with some advocates against corporate influences in medicine calling for the closure of HCA-affiliated EM programs. HCA now has 16 affiliated EM programs, the most of any hospital system, but is only responsible for 7 of the 57 programs opened in the past 5 years.5 Due to concerns regarding HCA’s rate of growth, ACEP met with HCA leadership last year and successfully advocated against the opening of a new EM program in one large urban center. Though only a first step, it does suggest organizational advocacy could play a role in ensuring responsible expansion.
Some critics of corporate influences in medicine have suggested it is the ACGME’s responsibility to close programs associated with for-profit hospitals. One difficulty with this suggestion is that neither the ACGME nor any other regulatory body currently exists to monitor or accredit residencies based on job market concerns or the hospital’s business model. In fact, the ACGME is legally restricted from considering these factors in its accreditation process due to antitrust regulations.6
The ACGME could increase residency standards such as procedure numbers and faculty requirements in order to ensure the quality of residencies remains high despite growth. This may inadvertently reduce the number of programs or downsize programs if they cannot meet more stringent ACGME standards.
As a parallel, orthopedic programs and positions have expanded more slowly than EM’s. This is in part due to their ACGME requirements, which mandate, for example, that orthopedic residents log at least 1,000 procedures and 200 pediatric procedures to graduate.7 In contrast, EM residents are only required to log 45 adult medical resuscitations and 35 intubations to graduate.8
Last year, the EMRA Board of Directors submitted recommendations to the ACGME specifically requesting that certain EM residency requirements be increased. As of 2023, the ACGME is actively reviewing these recommendations.
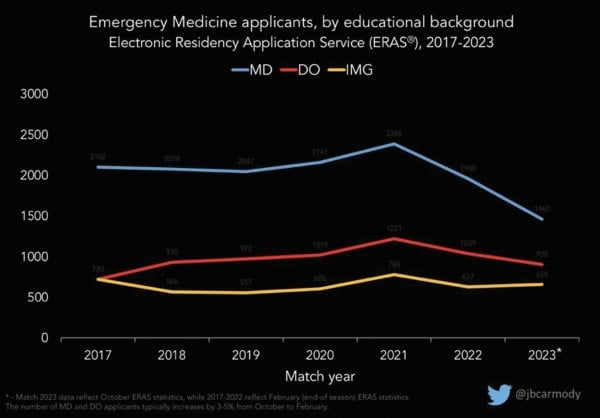
Graphs courtesy of Bryan Carmody, DO. Used with permission.
Solutions
First and foremost, EM physicians at every level of training must accept that, unlike the rapid improvements we see when saving our patients’ lives, this is not an issue we will fix immediately, or even within the next year. But there are strategies we can all adopt, regardless of our career stage, to strengthen our specialty.
On a personal level, each and every emergency physician can strengthen EM recruiting today by practicing awareness around the messaging we give students on shift and online. Opportunities to mentor, educate, and celebrate EM are available to anyone working with students in the ED or active on social media. Each EM-bound medical student also has a vested interest in bringing their dedicated, patient-centered colleagues into the specialty. EMRA’s medical student leaders advocate as passionately for the specialty as our most seasoned alumni.
At medical schools, third-year EM clerkships must be accessible and meaningfully incorporate students into the team. Throughout acting internships, students need excellent, direct feedback that allows them to reach their greatest potential, reducing their risk of going unmatched. When it comes to the application process, programs unfilled by the Match must adapt quickly and consider interviewing applicants they previously would not have considered.
Regarding residency growth, program leaders at established programs have a duty to consider their communities’ long-term needs when considering expansion. There is no regulatory body that currently exists to regulate expansion of programs. In 2023, however, the ACGME is reviewing EM program requirements. I have met with ACGME leadership to express our concerns and share our view that EM is overdue for a strengthening of our qualifications, procedural skills, and program support.
Moving forward, we must communicate to medical students and our colleagues that we recognize EM is in a challenging position, but we are tackling it head-on. We are united in initiatives like CORD’s Match Taskforce, composed of leaders across EM organizations. EMRA is also addressing it in our own ways: EMRA held an EM Match Open Forum at our spring meeting of the Representative Council in which residents from dozens of EM programs convened to learn about the Match, share their experiences at a wide range of programs, and discuss solutions. I then shared those experiences with other EM organizations and the ACGME. Our goal is to keep the quality of our training high — regardless of the age or business model of our EDs.
And as individuals, we can start today by celebrating the wins: the gratification in resuscitating a patient in distress, the accomplishment that comes from improving care in your emergency department, the hope that a new class of emergency physicians brings, and the ability to take care of anyone, anything, anytime. These wins are what drew me to emergency medicine, and what will draw in the next class of residents as well.
Jessica Adkins Murphy, MD
EMRA President
References
- Carmody B. Is there an emergency for emergency medicine? The Sheriff of Sodium; 2022. Available at: https://thesheriffofsodium.com/2022/10/24/is-there-an-emergency-for-emergency-medicine/. Accessed March 17, 2023.
- NRMP. Advance Data Tables 2023 Main Residency Match. NRMP; 2023. Available at: https://www.nrmp.org/wp-content/uploads/2023/03/2023-Advance-Data-Tables-FINAL.pdf. Accessed March 22, 2023.
- Marco CA, Courtney DM, Ling LJ, et al. The Emergency Medicine Physician Workforce: Projections for 2030. Ann Emerg Med. 2021;78(6):726-737. doi:10.1016/j.annemergmed.2021.05.029
- Cai A. Unity, Purpose, and Passion: Influencing the Future of the EM Workforce. EMRA; 2022. Available at: https://www.emra.org/be-involved/be-an-advocate/working-for-you/2022-workforce-study-statement-cai/
- ACEP. Health Systems Affiliated with 3+ New EM Residency Programs. ACEP; 2021. Available at: https://www.acep.org/life-as-a-physician/workforce/health-systems-affiliated-with-3-new-em-residency-programs/
- Weinmeyer R. Challenging the Medical Residency Matching System through Antitrust Litigation. AMA Journal of Ethics; 2015;17(2):147-151. doi: 10.1001/virtualmentor.2015.17.2.hlaw1-1502. Available at: https://journalofethics.ama-assn.org/article/challenging-medical-residency-matching-system-through-antitrust-litigation/2015-02. Accessed March 18, 2023.
- ACGME. Orthopaedic Surgery Minimum Numbers. ACGME; 2014. Available at: https://www.acgme.org/globalassets/pfassets/programresources/260_ors_case_log_minimum_numbers.pdf. Accessed March 22, 2023.
- ACGME. Emergency Medicine Defined Key Index Procedure Minimums. ACGME; 2017. Available at: https://www.acgme.org/globalassets/pfassets/programresources/em_key_index_procedure_minimums_103117.pdf.


