The Patient
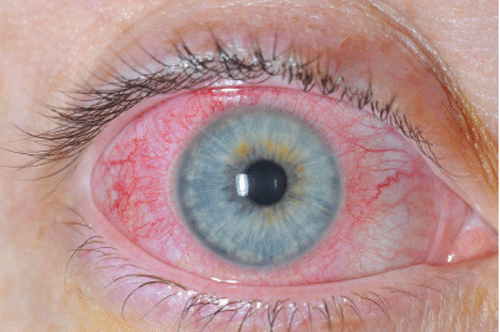
A 31-year-old female presents to the emergency department with 1 week of right eye pain, redness, excessive tearing, and photophobia. She denies any trauma, chemical exposures, or any change in visual acuity. She does wear contact lenses, but has been using them appropriately. She has no history of autoimmune disorders or inflammatory bowel disease, and has no skin ulcers, joint pain, or back pain. Her visual acuity is 20/20 in both eyes, but she is intensely photophobic on direct and consensual examination. Her extraocular movements are normal, and her gross examination is remarkable for the findings seen in the image provided. Slit lamp examination reveals no corneal fluorescein uptake, but there are 3+ cells in the anterior chamber. Her intraocular pressures are normal.
What is the diagnosis?
Diagnosis
This patient has anterior uveitis, which is an acute inflammation of the structures of the anterior chamber of the eye, including the iris. The eye examination reveals the presence of diffuse corneal injection with circumcorneal involvement, also known as a ciliary flush. Ciliary flush occurs because of injection of the episcleral vessels around the cornea, which is not seen in simple conjunctivitis. Patients with acute iritis should be seen by an ophthalmologist within 24 hours, and they are treated with topical cycloplegics and corticosteroids. Extreme caution should be used whenever topical corticosteroids are administered, and generally should only be utilized when recommended by an ophthalmologist. Iritis may represent the first clinical manifestation of systemic inflammatory disease. Primary care follow-up is appropriate for outpatient testing for underlying systemic etiologies.