Flaccid paralysis of the bilateral lower extremities in infants can be the presenting feature for a variety of diseases. This case follows the presentation and clinical course for an infant presenting to the ED with this chief complaint.
History
A 7-week-old previously healthy male was brought in for evaluation of decreased activity, a weak cry and refusal to feed. Parents reported leaving the infant in the care of a babysitter for approximately 10 hours on the day prior to presentation. While giving him a bath on the day of presentation, his mother noted that both of his legs appeared “dead.” Parents denied any history of trauma, fever, rhinorrhea, rashes, difficulty breathing, seizure-like activity, travel, or sick contacts. He had been feeding, voiding, and acting at baseline until the day prior. One week prior he was diagnosed by his pediatrician with oral thrush and diaper dermatitis and was prescribed nystatin topical and oral. He was born at term following an uncomplicated pregnancy and uneventful perinatal period. He had no known allergies, was circumcised, on no other medications, and had not yet received any immunizations.
Physical Examination
Vital signs in the ED were age-appropriate with the exception of a temperature of 38.10C, and a respiratory rate of 52 breaths per minute. The infant was well developed and well-nourished, but lethargic and ill-appearing with a weak cry. Nasal flaring with subcostal retractions were noted, but lung fields were clear to auscultation. Neurological examination revealed decreased spontaneous movement of both lower extremities with bilateral hypotonia, more pronounced on the right relative to the left. He had unrestricted passive range of motion and symmetric deep tendon reflexes with up going plantar reflexes bilaterally.
ED Course
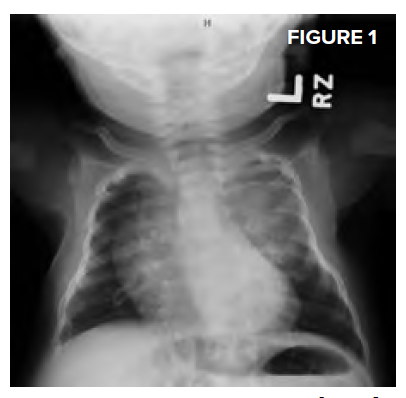
Complete blood count showed a white blood cell count of 13.5 K/ mm3, hemoglobin of 8.8 gm/dL, and a platelet count of 332 K/mm3. Differential count, reticulocyte count, and peripheral smear were unremarkable. Comprehensive metabolic panel, urinalysis, and electrocardiogram were unremarkable. CRP was elevated at 17.2 mg/L and albumin was low at 3.2 gm/L. Cerebrospinal fluid analysis demonstrated 243 nucleated cells with protein > 460 mg/dL. Blood, CSF, and urine cultures were obtained, and the patient was started on meningitic doses of ampicillin and cefotaxime. Chest radiograph showed an opacity over the left upper chest with a tapered appearance and splaying of the posterior 3rd-5th ribs, concerning for a paraspinal mass.
Final Diagnosis
Computed tomography of the thorax with contrast showed a 4.5 cm calcified left paraspinal mass with thinning and splaying of multiple ribs, with extension into the spinal canal from T3 through T6 and displacement of the airway and aorta (Figure 1 below). Magnetic resonance imaging showed a large mediastinal component (6.5 x 4.9 x 4.3 cm) with possible supraclavicular extension versus lymph node involvement (Figure 2 top right).

He was started on high-dose steroids, and an emergent thoracic laminectomy with tumor excision was performed. Final tumor pathology demonstrated poorly differentiated neuroblastoma and the patient was classified as stage 3 neuroblastoma, intermediate risk, based on the International Neuroblastoma Staging System.
Discussion
- Unexplained flaccid paralysis of the lower extremities in an infant should prompt further evaluation and the differential diagnoses are varied.
- Potential etiologies include infectious, inflammatory, traumatic (accidental versus non accidental), congenital and/or neoplastic causes.
- Neuroblastoma arises from the adrenal glands or follows the distribution of the sympathetic ganglia along the paraspinal areas from the neck to the pelvis; thus, neuroblastoma is likely to extend into the intra spinal space.
- Up to 50% of patients with intra-spinal tumour extension present with periph.eral neurologic deficits and neurological symptoms from compression of the nerve roots or the cord.
- Neuroblastoma is usually an incidental diagnosis, identified on imaging ordered for another indication (e.g. chest radiography for pneumonia as with our case).
- A normal CBC does not rule out infiltrative/neoplastic processes, and in the appropriate clinical setting, additional evaluation with CT or MRI is required.
Conclusion
ED physicians must be cognizant of the widely variable clinical presentation of neuroblastoma in children.



