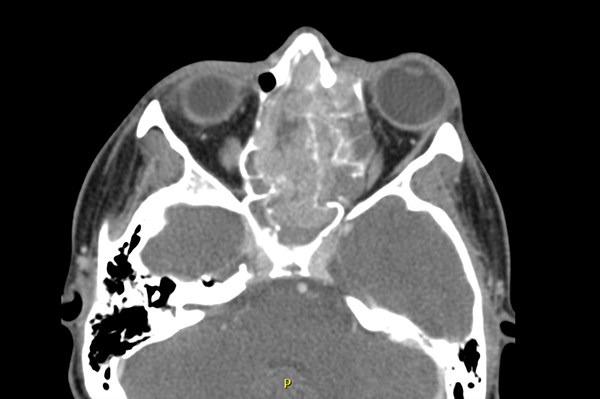
A 14-year-old male presented to the ED with a chief complaint of vision changes. For three months he had been seen by his pediatrician and diagnosed with recurrent sinusitis and upper respiratory infections. Upon ED presentation, he reported left eye swelling with blurred vision. He denied eye redness or pruritus, fever, or photophobia. His mother insisted that his left eye was swollen and “different” than the right eye. Vital signs were T: 36.5 C, HR: 83, BP: 129/81, RR: 19, SpO2: 100% on room air. Physical exam was remarkable for left eye proptosis, left eye discharge, limited upward and lateral movement of the left eye, and bilateral maxillary sinus tenderness. A CT of the orbits with and without contrast revealed a heterogenous mass in the left nasal cavity which extended upward into the anterior cranial vault and left maxillary sinus. He was admitted to the pediatric inpatient service with consultations to pediatric neurosurgery and pediatric hematology-oncology.
Discussion
Nasopharyngeal tumors are rare and their ED presentation is variable, ranging from benign symptoms such as rhinorrhea to more insidious clinical findings, including facial asymmetry or neurologic sequelae.
Tumors of the nasopharynx may be benign or malignant. Benign tumors include angiofibroma and craniopharyngioma.1 These primarily occur in children or young adults with the most common presenting symptoms being epistaxis and nasal obstruction.1
Malignant nasal tumors include nasopharyngeal carcinoma and may, even more rarely, be of neuroendocrine or neuroectodermal origin. Risk factors for carcinoma include EBV infection, which may spur malignant transformation of nasal epithelium.2 While rare in the continental US, incidence is highest in Tunisia, China, Southeast Asia, Alaska, and the Mediterranean basin.2 Nasopharyngeal carcinoma arises from epithelium of the fossa of Rosenmuller in the lateral nasopharynx and may metastasize to cervical lymph nodes, bone, lung, and mediastinum.2
Like the tumor in this case, neuroendocrine and neuroectodermal tumors of the nasopharynx are even less common. These are characterized as small, round blue cell tumors.3,4 Primary neuroendocrine neoplasms typically involve the lungs but rarely originate in the head or neck.3 These tumors have a penchant for highly aggressive behavior and prognosis is typically poor.3
Neuroectodermal tumors, such as esthenioneuroblastoma (ENB), arise from the olfactory nerve and can extend upward into the orbit and anterior cranial fossa.4 Peak incidence is in the second decade of life with a pediatric incidence of 0.1/100000.4 These historically follow an indolent course or are aggressive with fast growth and early metastatic spread.4
Nasopharyngeal tumors are exceedingly rare but their clinical presentation often includes symptoms commonly seen in the ED. These may include symptoms of more benign conditions, such as rhinitis or sinusitis. Many patients with tumors of the nasopharynx experience nasal obstruction, eye discharge, and rhinorrhea, which is often unrelieved by antihistamines. Benign tumors and carcinoma may present with recurrent epistaxis.1,2 Mass effect may contribute to more advanced symptomatology. Patients may experience voice changes as the tumor grows and begins to affect air movement through the involved nare. In patients with ENB, facial asymmetry may occur as the tumor enlarges as well as proptosis and visual field changes if the orbit or optic nerve are affected.4
A tumor of the nasopharynx may be considered in patients presenting with multiple ED visits for rhinorrhea, epistaxis, facial asymmetry, ocular symptoms, and cranial nerve palsies. Diagnostic work up should be guided by clinical exam. Imaging may include CT of the head, facial bones, sinuses, and orbits.2 Depending on availability MRI is a useful modality for evaluation of soft tissues of the head and neck if tumor is found on CT.2
ED management of nasopharyngeal tumors consists of a two-pronged approach: stabilization and early consultation. Airway must take first precedence. Theoretically, in the case of large and possibly hemorrhagic nasopharyngeal masses, ED physicians must include an airway management plan in addition to timely consultation.
Malignancies of the nasopharynx are often high-grade and aggressive.2-4 Therefore, prompt consultation to hematology-oncology and ENT must be made. If there is invasion into the anterior cranial fossa, as seen in this case, discussion must be held with neurosurgery. Final diagnosis depends on formal biopsy. Treatment includes a combination of chemotherapy and radiation with surgical resection.2,3
Case Conclusion
Pediatric ENT and oncology were consulted. Biopsy revealed a small, round blue cell tumor of neuroendocrine or neuroectodermal origin. He received combination chemotherapy and was diagnosed with Li-Fraumeni syndrome, a rare familial cancer syndrome that occurs due to loss of function mutations in tumor suppressor genes. After chemotherapy tumor mapping revealed that the tumor is necrotic. ENT/neurosurgery team believe that surgical intervention is not necessary. He is followed by pediatric-oncology and continues to receive chemotherapy.
References
1. Mohanty S, Gopinath M, Subramanian M. Benign Tumors of Nasopharynx – Revisited. Indian J Otolaryngol Head Neck Surg. 2013;65(1):22-25.
2. Brennan B. Nasopharyngeal carcinoma. Orphanet J Rare Dis. 2006;1:23.
3. Azevedo D, Rios E, Vendeira L, Sarmento C. Small cell neuroendocrine carcinoma of the nasopharynx: a rare case report. Autops Case Re. 2017;7(1):31-35.
4. Kumar R. Esthesioneuroblastoma: Multimodal management and review of literature. World J Clin Cases. 2015;3(9): 774-778.