Accidental poisonings account for nearly 70,000 pediatric visits to the ED every year. Which ingestions might be fatal, even at small doses? How will you know what to check in an asymptomatic patient?
Background
A 2-year-old is brought into your ED after her grandmother noticed some of her pills were missing. The grandmother is worried her granddaughter may have taken the pills. The physical exam and vital signs are normal. The grandmother’s medications include glipizide and lisinopril.
How long do you observe the patient? What worrisome exam or diagnostic findings should you look for?
In 2017, almost half of pediatric ingestions were for unintentional exposures in children less than 5 years old.1 Approximately 70,000 ED visits are for unintentional ingestions each year.2 Most ingestions are benign because of the small quantity/dose and benign nature of the material ingested. However, it is important to know which ingestions can be fatal in infants and toddlers, even at small doses, and what exam and diagnostic findings to look for.
Furthermore, on initial exam, the child may be completely asymptomatic with normal vital signs and labs. It is important to get a good history and observe or admit them based on the potential ingestion and not the exam findings or labs. This is especially true for slow or sustained/extended release medications.
Caveat:
- Although beta blockers are not considered in the “one pill kill” category, it is important to understand the pathophysiology of the beta blockers and its presentation. Thus, it is included in this section.
Calcium Channel Blockers (CCBs) and Beta Blockers (BBs)
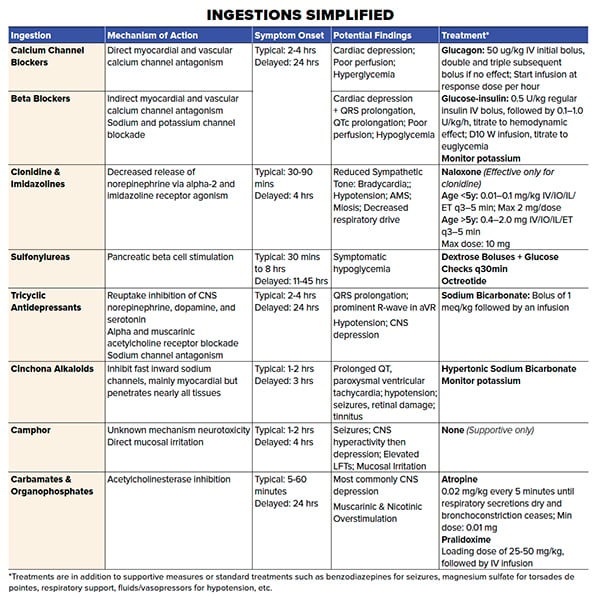
Both CCBs and BBs can lead to cardiogenic shock by antagonizing myocardial and vascular calcium channels, resulting in decreased contractility (inotropy and chronotropy) and hypotension resulting from decreased vascular tone. Although CCBs cause direct calcium channel blockade, and BBs cause indirect calcium channel blockade, it is very difficult to differentiate a CCB versus BB ingestion based on presentation. Although, CCB toxicity tends to have hyperglycemia as part of the patient presentation while BBs do not.
CCBs can be fatal at a dose of 15 mg/kg consistent with exploratory ingestions, with the largest dose coming in 360 mg instant release.3 CCBs are type IV antiarrhythmics and act on the AV node, resulting in heart block (PR prolongation on EKG), bradydysrhythmias, hypotension, and potentially heart failure. In 2004, a case report illustrated the dangers of CCBs after a 14-month-old girl died after ingesting just one nifedipine 10-mg tablet.4
BBs are almost never fatal in exploratory ingestions but are important to consider in an older pediatric patient with suicidal intentions. BBs are type II antiarrhythmics and act on the SA and AV nodes, resulting in sinus bradycardia, PR prolongation and bradydysrhythmias similar to CCB toxicity. However, some BBs can result in intraventricular conduction delay (QRS prolongation) and QTc prolongation via sodium and potassium channel blockade similar to type I/III antiarrhythmics.5 Furthermore, BBs are lipophilic and can have a large distribution and extended effects.5 Propranolol is most lipophilic, allowing it to cross the blood-brain barrier and result in seizures. Propranolol, along with sotalol, is most likely to cause conduction delays as well as wide complex tachycardias.5
Due to CCBs and BBs effects of bradycardia and bradydysrhythmias there is a theorized increased risk of early cardiogenic shock and heart failure in children, who are highly dependent on Heart Rate (HR) for Cardiac Output (CO=Stroke Volume x Heart Rate).
Exam findings in symptomatic patients are due to myocardial suppression and vascular relaxation resulting in fatigue, poor feeding in infants, lethargy, poor perfusion (poor capillary refill, faint pulses), etc. Patients will be bradycardic and hypotensive with little response to atropine/fluids and even cardiac pacing. CCBs may lead to hyperglycemia due to impaired insulin release, while BBs may lead to hypoglycemia due to increased insulin release.4
Treatment is targeted at the symptoms, vital signs, and diagnostic findings. Administer sodium bicarbonate for QRS widening and magnesium sulfate for QTc prolongation. Treat cardiogenic shock with fluids, atropine, and vasopressors in both CCB and BB ingestions. Consider early IV glucagon in BB overdose (50 mcg/kg IV initial bolus) with doubling the dose and redosing Q10-20mins.4 If efficacious, then start a drip of the effective dose.4 For example, if a 1-mg dose is effective start a drip at 1 mg/hr.
Pearl: Always give glucagon with an antiemetic to avoid airway emergency due to aspiration.
With CCB toxicity you can try giving IV calcium. However, if nothing is working then you must resort to hyperinsulinemia-euglycemia therapy, which combines an insulin infusion with dextrose, as needed, to maintain normal blood glucose. Give an IV insulin bolus at 1 IU/kg along with 10 or 25 g dextrose bolus.4,5 Then start an insulin drip at 0.5 IU/kg/hr with IV glucose replaced as needed with Accu-Cheks Q30 min within a range of 100-250. It is vital to get a potassium level prior to initiation and to monitor potassium levels closely. If the patient is still unresponsive, then intralipid therapy and/or Extracorporeal Membrane Oxygenation (ECMO) may be considered.5
IV calcium is typically used for CCB overdose, not BB overdose. Glucagon is used for BB overdose, but not CCB overdose. In addition, for CCB overdose, standard pressures can also be utilized. HIE therapy works for both CCB and BB.
Pearl: CCBs or BBs should be observed for at least 24 hours due to possible long-acting formulations.
Alpha-Adrenergic and Imidazoline Agonists
Alpha-2 and imidazoline receptor agonists commonly involved in toxic ingestions include clonidine, nasal decongestants (oxymetazoline, tetrahydrozoline, and xylometazoline), and glaucoma agents (brimonidine, apraclonidine).4 All of these agents can have a delayed presentation of up to 4 hours, but typically present within 30-90 minutes and can have persistent effects for 1-3 days. Agonistic effects at the centrally (CNS) located alpha 2 receptor result in decreased release of norepinephrine and, therefore, globally reduced sympathetic tone.4 This results in bradycardia and hypotension, but it can also result in altered mental status, miosis, and decreased respiratory drive similar to an opioid toxidrome.4
Pearl: Toxic effects may be delayed up to 4 hours and may persist for 1 to 3 days
Hypotension is managed with fluids/vasopressors, bradycardia is managed with atropine/pacing, and bradypnea/decreased respiratory drive is managed with naloxone/positive pressure ventilation/intubation.4 The dose of naloxone is 0.1 mg/kg, up to a total of 10 mg and may be beneficial for clonidine toxicity, but less so for imidazolines.4
Sulfonylureas
Sulfonylureas are insulin secretagogues used in treating type 2 diabetes. They stimulate pancreatic beta cells to secrete insulin.4,6 Time of onset is within 30 minutes, while peak concentrations are reached at 4-6 hours with long-term effects up to 24 hours.4,6
Sulfonylureas have narrow therapeutic indexes with small doses of just 0.1 mg/kg resulting in severe hypoglycemia in children.3,4,6 Hypoglycemia has been reported in children who have ingested just 1 tablet of chlorpropamide, glipizide, or glyburide.4,6 In pediatric patients, hypoglycemia is typically observed within 8 hours of ingestion.3,4,6 However, there are reports of delayed onset (11-45 hrs) and recurrence up to 30-70 hours after ingestion.3,4,6
Hypoglycemia is commonly referred to as the syphilis of metabolic disorders and can mimic a wide array of presentations. Exam findings can include irritability, poor feeding, lethargy, seizures, altered mental status, coma, etc.3 Vitals may be normal or demonstrate bradycardia, hypotension, or irregular respirations.3 Therefore, it is important to always check a glucose on every patient with any of the above presentations and have ingestion on your differential for unexplained hypoglycemia. Typically, dextrose boluses are sufficient to manage hypoglycemia. However, octreotide can be useful for patients with refractory hypoglycemia.6
Confirmed or suspected sulfonylurea ingestions may require 24 hours of observation with glucose monitoring. Therefore, it is easy to justify admission for observation.
Pearl: Patients with sulfonylurea ingestion typically require 24 hour observation
Tricyclic antidepressants (TCAs)
TCA ingestions can be deadly and easy to miss. They have a narrow therapeutic index and long half-life (often > 24 hours). They act by inhibiting the reuptake of norepinephrine, dopamine, and serotonin in the CNS and also block alpha and muscarinic (acetylcholine) receptors, which can result in reflexive tachycardia.3,7 Furthermore, they act as sodium channel antagonists in cardiac myocytes, which can result in dysrhythmias.3,7
Exam findings can be normal or include lethargy, poor feeding, coma, and seizures. Vitals may be normal or include tachycardia, bradycardia, and hypotension.3 Tachycardia without any other findings responds to benzodiazepines.7 Hypotension from TCAs will typically respond to fluids but may need vasopressors to work against the alpha antagonistic effect of TCAs.7
The most dangerous effect of TCA toxicity is due to cardiac sodium channel antagonism and resultant QRS prolongation (>0.10 secs) and prominent R-wave in aVR, which can lead to dysrhythmias and cardiac arrest.4,7 Sodium bicarbonate is the treatment of choice for QRS prolongation and should be given promptly to any patient who is suspected of having a TCA overdose with EKG changes. It is given as a bolus of 1 mEq/kg followed by an infusion.4,7 Because of the long half-life of TCAs, patients with suspected TCA ingestion require 24 hour observation with continuous cardiac monitoring.4,7 Patients who are alkalotic should be given hypertonic saline, which competes with TCAs’ antagonism at cardiac sodium channels.
If a patient with TCA ingestion continues to be symptomatic, both ECMO and lipid emulsion therapy can be considered and maybe live saving.
Pearl: Suspected TCA toxicity with EKG changes of QRS prolongation (>0.10 secs) should be emergently treated with Sodium Bicarbonate.
Cinchona Alkaloids
Cinchona Alkaloids include antimalarials like quinidine and chloroquine, which are commonly prescribed at doses up to 600 mg per tablet and can be fatal at doses of 20 mg/kg, a mere third of a tablet for a 10 kg child.8,9 Have a high suspicion of ingestion of antimalarials if there is a history of recent travel or planned travel, as patients or family may be on malarial prophylaxis.
Cinchona Alkaloids are Class 1A antiarrhythmic agents and inhibit cardiac myocyte sodium channels, which results in prolonged QRS and QT intervals and ventricular tachydysrhythmias.
Acute toxicity can present with confusion, syncope, palpitations and hypotension.9,10 Cinchona Alkaloids can also cause retinal damage and present with blurry vision.9,10 Other potential presentations can include headache, hearing impairment, flushing, hypersensitivity reactions such as fever, rash, blood dyscrasias, hepatitis, tinnitus, and gastrointestinal upset.10 Maximum concentrations will occur within 1-2 hours of oral intake.9,10
Pearl: Think Cinchona Alkaloids when a patient presents with blurred vision and/or hearing impairment in the setting of an arrhythmia
Management of acute intoxication includes magnesium sulfate, potassium, and overdrive pacing for QT prolongation and Torsades de Pointes.10 Activated charcoal readily absorbs quinine and may be considered early after ingestion, with standard pediatric dosing of 0.5-1 gm/kg PO.11 Sodium bicarbonate should be given for prolonged QRS interval or heart block to antagonize the inhibitory effects on sodium channels, with a target pH of 7.45-7.50.11 Be sure to monitor and correct potassium when administering bicarbonate. ECMO should be considered in any patient with continued cardiac depression not responding to treatment.
Camphor
Camphor ingestions often come from household products such as Vaporub®, Orajel™, and Tigerbalm® used as a cough suppressant and for mouth and muscle pain, respectively. Due to rapid absorption, effects can occur within 5-20 minutes, although typical onset is closer to 1-2 hours.11,12 A single teaspoon (~5 mL) can be fatal with the doses available at 550 mg/tsp; therefore, high suspicion and immediate action is crucial.9 The exact mechanism of neurotoxicity is unknown, but the concurrent liver toxicity seems to transpire through a mechanism similar to Reye Syndrome. Direct mucosal irritation can cause oropharyngeal burning, abdominal pain, vomiting, and diarrhea.12,12 Seizures are often the first sign of toxicity. However, CNS symptoms can transpire in 2 phases, with an initial phase of agitation, anxiety, hallucinations, hyperreflexia, and myoclonus and a second phase of lethargy, coma, and respiratory depression.4,9,12
Pearl: Keep camphor ingestion on your differential when considering elevated LFTs, altered mental status, neurologic changes with subsequent respiratory depression. Look out for its unique potent smell (mothball-like odor).
Treatment is supportive. Manage respiratory and CNS depression with positive pressure ventilation/intubation. Seizures are often short-lived and may not require any active intervention, but any prolonged seizures should be treated with benzodiazepines.4,12 Asymptomatic patients, 4 hours post-ingestion, can be safely discharged home.
Pearl: Asymptomatic patients, 4 hours post-ingestion, can be safely discharged home.
Carbamates & Organophosphates
Organophosphates and carbamates are still found commonly in insecticides. Although less commonly ingested, they have the potential of being fatal in children in a single swallow.12 Depending on the route of exposure, the effects can take place within minutes.11 These poisons act as acetylcholinesterase inhibitors, leading to excessive stimulation of muscarinic and nicotinic receptors. Unlike in adults, children manifest commonly with CNS symptoms, such as seizures, coma, and respiratory failure.12
Treatment should target each patient’s specific symptoms. For wheezing, airway secretions, and other muscarinic symptoms, administer atropine 0.02 mg/kg every 5 minutes until respiratory secretions dry and bronchoconstriction ceases.12 For seizures, follow your normal seizure algorithm; however, consider atropine as it can fix the underlying problem. Also give concurrent pralidoxime chloride (2PAM) with atropine in all organophosphate poisonings. 2PAM prevents “aging” (irreversible inhibition) of acetylcholinesterase, primarily, at the neuromuscular junction. It is not helpful for carbamate poisoning.
If asymptomatic on arrival, children should be monitored for at least 4 hours before considering discharge.12 Typically symptoms will be seen within the first hour, and most agents will cause symptoms within 8 hours at most.11 However, lipophilic agents such as fenthion, or those like malathion that require metabolic activation, may have a delayed presentation up to 24 hours.11 Therefore, the observation time should be based on the pharmacokinetics of each agent.
Pearl: Tachycardia is not a contraindication for atropine use.
TAKE-HOME POINTS
- Do not underestimate ingestions; a child who comes in looking well can quickly become unresponsive and in shock.
- Investigate the type of ingestion in order to appropriately disposition the patient, as some long-acting agents can present many hours after ingestion.
- When presented with a critically ill pediatric or adult patient, do not underestimate the possibility of ingestion, as targeted treatments may be the difference between life and death.
References
- Gummin DD, Mowry JB, Spyker DA, Brooks DE, Osterthaler KM, Banner W. (2018). 2017 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 35th Annual Report. Clin Toxicol (Phila). 2018;56(12):1213-1415.
- Schillie SF, Shehab N, Thomas KE, Budnitz DS. Medication overdoses leading to emergency department visits among children. Am J Prev Med. 2009;37:181-187.
- Bar-Oz B, Levichek Z, Koren G. Medications that can be fatal For a toddler with one tablet or teaspoonful: a 2004 update. Pediatr Drugs. 2004;6(2):123-126.
- Michael JB, Sztajnkrycer MD. Deadly pediatric poisons: nine common agents that kill at low doses. Emerg Med Clin North Am. 2004;22(4):1019-1050.
- Khalid MM, Hamilton RJ. Beta-Blocker Toxicity. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018.
- Klein-Schwartz W, Stassinos GL, Isbister GK. (2016). Treatment of sulfonylurea and insulin overdose. Br J Clin Pharmacol. 2016;81(3):496-504.
- Kerr GW, McGuffie AC, Wilkie S. Tricyclic antidepressant overdose: a review. Emerg Med J. 2001;18:236-241.
- Travassos M, Laufer MK. (2019). Antimalarial drugs: An overview. UpToDate, 2019.
- Karb R. One Pill (or Sip) Can Kill. American College of Emergency Physicians, Toxicology Section, 2016. Available at: https://www.acep.org/how-we-serve/sections/toxicology/news/march-2016/one-pill-or-sip-can-kill/.
- Kim SY, Benowitz NL. Poisoning due to class IA antiarrhythmic drugs. Quinidine, procainamide and disopyramide. Drug Saf. 1990;5(6):393-420.
- Goldfrank L, Nelson, L. Goldfrank's Toxicologic Emergencies. 9th ed. New York: McGraw-Hill Medical, 2011.
- Eldridge DL, Mutter KW, Holstege CP. An evidence-based review of single pills and swallows that can kill a child. Pedatr Emerg Med Pract. 2010;7(3):1-16.



