It is important to consider that acute urinary retention can be a subtle clue of a neurologic process warranting emergent CT imaging to rule out vertebral fracture and MRI to rule out spinal cord compression.
Case
A 65-year-old female with a past medical history of borderline personality disorder, bipolar I disorder, and chronic obstructive lung disease presented to a community ED with bilateral flank pain. She reported discomfort ongoing for 2 weeks and progressively worsening over the past 3 days. She had not urinated in 2 days and had not had a bowel movement in over 7 days. She denied fevers, chills, lower extremity weakness, or new medications. Her initial physical exam was notable for a distended and diffusely tender abdomen, bilateral flank tenderness, and no midline spinal tenderness. Bladder scan at bedside revealed a significantly distended urinary bladder. Neurologic exam demonstrated equal strength and sensation to the bilateral upper and lower extremities, no saddle anesthesia, and normal rectal tone. Her genitourinary exam was also normal. A Foley catheter was inserted and resulted in over 2 L of urine within the first hour. Catheter insertion relieved the patient’s abdominal distention, but not her flank pain. Labs were significant for leukocytosis of 17.0 with a neutrophil predominance, hypokalemia of 3.2 mmol/L, and a mildly elevated alkaline phosphatase of 132 IU/L. The remainder of her labs and imaging, including lactate, urinalysis, and CT abdomen and pelvis, were unremarkable. CT lumbar spine reconstruction was ordered after it was revealed the patient had slipped and fell onto her back two days prior while attempting to sit down on a chair. Ultimately her reconstruction images were unremarkable. Due to concern for spinal pathology causing her new-onset urinary retention, the patient was transferred to the nearest academic center for neurologic evaluation and emergent MRI.
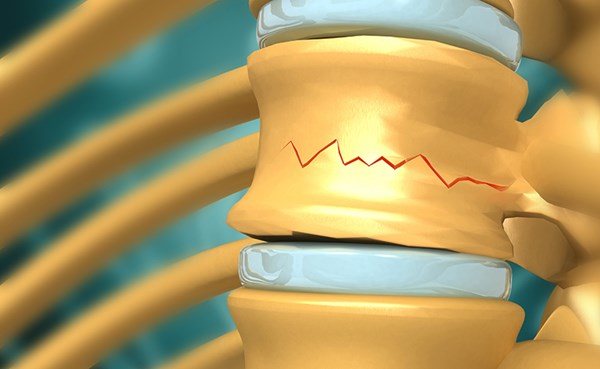
At the academic medical center neurology was consulted and again noted a normal neurologic exam. Additionally, reflexes were normal and symmetric in all extremities, without clonus, except for the right patellar reflex, which was absent in the setting of a prior knee replacement. Plantar reflexes showed withdrawal response bilaterally. Cervical and thoracic spine CT imaging revealed an acute burst-morphology fracture of the T8 vertebral body with involvement of the bilateral facets, making it an unstable 3-column injury (Image 1).

Image 1. Unstable 3-column injury in urinary retention patient
Radiology noted severe fragmentation with retropulsion of fracture fragments into the spinal canal. MRI showed retropulsion resulting in severe spinal canal narrowing, advanced T8-T9 neural foraminal narrowing, and cord compression at this level with evidence of developing myelopathy (Image 2).
 Image 2. MRI showing developing myelopathy
Image 2. MRI showing developing myelopathy
Additionally, there was found to be marrow edema within the anterosuperior and posterior T9 vertebral body and bilateral pedicles indicating additional injury sites. There was also presumed disruption of the anterior and posterior longitudinal ligaments at the T8 level with evidence of interspinous ligament strain from approximately T6-T10. MRI found no evidence of distal cord or cauda equina compression. Given the unstable nature of the patient’s fracture she was taken emergently for T6-T10 posterior spinal fusion, T8 laminectomy, and left trans-pedicular open reduction of fracture and ventral cord compression.
Discussion
Acute urinary retention (AUR) is rare in women, with an occurrence rate estimated at 3 cases per 100,000 women per year.1 Similar to men, outflow obstruction is the most common cause. Obstruction in females typically manifests secondary to pelvic organ prolapse or pelvic mass. Medications can induce AUR; while anti-cholinergic and sympathomimetic medications are most common, the list includes anti-depressants, muscle relaxers, and anti-psychotic medications.1-2
As evidenced by this case, AUR can also have a neurologic etiology; spinal cord injuries from trauma, epidural abscess or metastasis, stroke, or demyelinating disease. In a recently published systematic review of the diagnostic accuracy of 84 red flag signs and symptoms, new urinary retention or bladder/suprapubic fullness on physical exam were shown to have positive likelihood ratios of 7.0 (95% CI: 1.9-26.0) and 40.2 (95% CI: 1.6-979.1), respectively, for serious spinal pathologies (e.g. vertebral fractures, cauda equina compression, cancer, and infectious disorders).3
We commonly remember to evaluate for saddle anesthesia when seeking to identify spinal pathology, and for good reason, as the study identified a positive likelihood ratio (7.0; 95% CI: 1.4-36.0) associated with disturbance of saddle sensation on physical exam. However, as this case demonstrates, serious spinal pathology can present in the absence of saddle anesthesia, with the presence of smaller red flag symptoms. As such, it is important to consider that acute urinary retention can be a subtle clue of a neurologic process warranting emergent CT imaging to rule out vertebral fracture and MRI to rule out spinal cord compression.
References
- Barrisford GW and Steele GS. Acute Urinary Retention. UpToDate. (2019) Retrieved May 3, 2020. https://www.uptodate.com/contents/acute-urinary-retention.
- Verhamme KM, Sturkenboom MC, Stricker BH, Bosch R. Drug-induced urinary retention: incidence, management and prevention. Drug Saf. 2008;31(5):373-88.
- Galliker G, Scherer DE, Trippolini MA, Rasmussen-Barr E, LoMartire R, Wertli MM. Low back pain in the emergency department: prevalence of serious spinal pathologies and diagnostic accuracy of red flags. Am J Med. 2020;133(1):60-72.