How to Match in EM: New Evidence
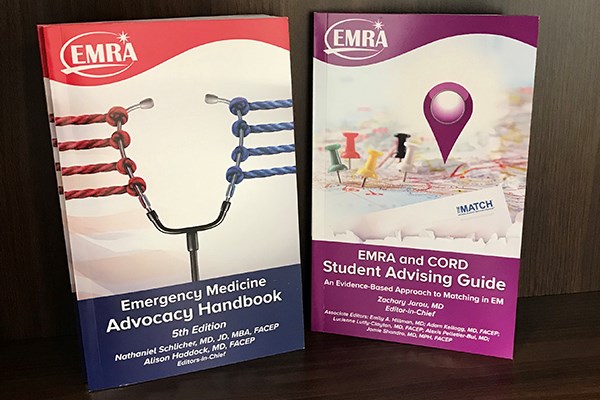
If any medical student has ever asked you for advice — or if you need advice yourself — then you must read the soon-to-be-released EMRA and CORD Student Advising Guide: An Evidence-Based Approach to Matching in EM.
This resource remakes EMRA's Medical Student Survival Guide into a primer for matching into the specialty, based on current evidence. How many audition rotations should you do? How do you line up SLOEs? How many interviews do you really need in order to match? What factors actually matter most in the process? Get advice based on analyses of recent match results, current literature, and surveys completed by the decision-makers in the specialty.
Many thanks to all the chapter teams — a faculty member, resident, and student member each collaborated to produce these chapters. Special recognition goes to editor-in-chief Zach Jarou, MD, and the Student Advising Guide senior editorial team — Emily Hillman, MD; Adam Kellogg, MD, FACEP; Lucienne Lutfy-Clayton, MD, FACEP; Alexis Pelletier-Bui, MD; and Jamie Shandro, MD, MPH, FACEP. These six physicians, all members of the CORD Advising Students Committee in Emergency Medicine, dedicated months to developing the Student Advising Guide, focusing on ways to mitigate the stress, anxiety, and expense of the match process. The book will be included in EMRA student member kits and will be posted online.
Advocacy in Focus
As health policy heats up on topics ranging from reimbursement practices to firearm injury research, it's more important than ever for emergency physicians to understand and exercise their advocacy abilities. Fortunately, EMRA can help. The Emergency Medicine Advocacy Handbook, 5th edition, will be released in conjunction with the ACEP Leadership & Advocacy Conference in May. This resource, which will also be posted online and presented as an audio book, lays the foundation for advocacy knowledge in the specialty. The book puts today's health care policy climate into context and offer insight on how the changing political landscape can affect emergency physicians and their patients. Editors-in-chief Nathan Schlicher, MD, JD, MBA, FACEP, and Alison Haddock, MD, FACEP, along with associate editor Rachel Solnick, MD, MSc, led a team of more than 90 emergency physicians, residents, and medical students in developing this edition.
US Acute Care Solutions provided an educational grant to help fund the book because the importance of advocacy is paramount, according to L. Anthony Cirillo, MD, FACEP, the company's director of Clinical Health Policy & Legislative Advocacy.
"The impact of policymaking on the lives of physicians and our patients is difficult to overstate," Dr. Cirillo said. "This is why US Acute Care Solutions' commitment to advocacy is so strong — because it is no exaggeration to say lives depend on it."
Free Service Can Help with Moving
EMRA alumni member Arun Ganti, MD, MPHS, FAWM, has devised a new service to help defray the cost of moving.
"The idea stems from my own experience moving for residency," Dr. Ganti said. "I experienced the benefits of having a shared move firsthand, and I'm hoping to re-create this for others who are in the same situation."
Called Backlode, the service is free and straightforward:
- Sign up at backlode.com by providing your email address, the cities you're moving from/to, and the desired time frame for your move.
- Browse the Backlode database to look for users with whom you can share a move. (All email addresses will be kept private.)
- Contact a moving company of your choice and negotiate a rate.
2019 Main Residency Match Breaks Records
The 2019 Main Residency Match is the largest in the history of the National Resident Matching Program.® A record-high 38,376 applicants submitted program choices for 35,185 positions, the most ever offered in the Match. The number of available first-year (PGY-1) positions rose to 32,194, an increase of 1,962 (6.5%) over 2018. The influx of positions is due, in part, to the increased numbers of osteopathic programs that joined the Main Residency Match as a result of the ongoing transition to a single accreditation system for graduate medical education programs.
The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools.
Emergency medicine programs offered 2,488 first-year positions, 210 more than in 2018, and filled all but 30. The overall fill rate was 98.8%, and 65.0% were filled by U.S. allopathic seniors. Since 2015, the number of EM positions has increased by 667, or 36.6%, driven in part by AOA programs entering the NRMP Match.
ABEM Drops CME Requirement
ABEM has removed the MOC requirement that physicians attest to completing an average of 25 CME credits every year. The American Board of Medical Specialties (the umbrella organization for specialty boards) approved this change for ABEM because LLSA activities are essentially CME activities for which CME credit can be claimed.
Eliminating this MOC requirement is one more way that ABEM is working to lessen the burden for physicians while maintaining the value of certification.