Vague neurologic symptoms, including impaired speech, can be difficult to diagnose and – for female patients – dismissed as behavioral.
But commonly prescribed medications such as SSRIs may be a cause of movement disorders and speech disturbance. This case of adult-onset stuttering illustrates the importance of a thorough history and an open-minded approach.
Case
A 23-year-old patient with a history of depression, attention deficit hyperactivity disorder (ADHD), hyperlipidemia, and diabetes presented to the ED with a 2-week history of tremor and a new symptom of stuttering.
She first noticed the stuttering while trying to have a conversation with her manager 2 days prior to the ED visit and reported associated symptoms of difficulty forming sentences, confusion, and bilateral lower extremity weakness that had gradually worsened since the time of onset. The patient had not experienced fever, cough, chills, nausea, vomiting, diarrhea, shortness of breath, chest pain or abdominal pain. Vital signs were as follows: blood pressure 113/79 mmHg, pulse 63 beats/min, respiratory rate 17 breaths/min, and temperature 37°C.
Physical examination showed a patient in no distress. Cardiovascular, respiratory and abdominal examination was unremarkable. Cranial nerves II-XII were intact. Motor strength was 5/5 in all extremities. Sensation to light touch was intact. Reflexes were 2+ in all extremities. There was no clonus noted.
The patient was ambulatory with a normal gait. Pronator drift and Romberg sign were negative, and no nystagmus was observed. Assessment of the patient’s speech revealed an obvious stutter that was difficult to control. When the patient was asked to lift her head upwards, the emergency physician noted a tremor and titubation on extension of the neck.
ED evaluation included blood glucose, CBC with differential, CMP, HCG, CK, urinalysis, CT brain, MRI brain (Figure 1), and MRI cervical spine. Laboratory results were within normal limits aside from a very minimal leukocytosis at 10.96 and hemoglobin of 15.3 that was normocytic. There was no evidence of renal dysfunction, transaminitis, or anion gap acidosis.
Figure 1. MRI-brain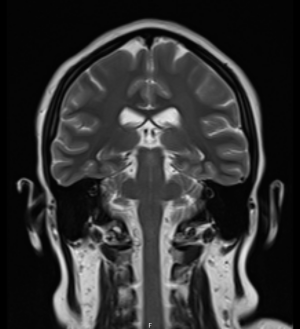
CT imaging was unremarkable. MRI of the brain with and without contrast showed no acute intracranial disease. MRI of the cervical spine showed no evidence of abnormal cord signal or enhancement.
The patient later revealed she was taking sertraline to manage depression, and her dose of 50 mg per day was increased to 100 mg a few days before symptoms started.
Discussion
Movement and speech disorders are associated with multiple medications. Extrapyramidal symptoms (EPS) include motor dysfunctions such as dystonia, akathisia, parkinsonism, tremor, and tardive dyskinesia. Drug-induced parkinsonism encompasses a wide array of symptoms including tremor, rigidity, and/or bradykinesia. EPS commonly present in patients taking dopamine-blocking drugs; however, they can occur with other psychotropic medications, including antidepressants.1 The pathogenesis of parkinsonism has been extensively studied in the setting of antipsychotic and dopamine blocking agents; however, cases have been documented with selective serotonin reuptake inhibitor (SSRI) use as well. Common risk factors for drug-induced parkinsonism are female gender, older age, current or prior use of antipsychotic medications, and prior history of movement disorder.2
The connection between SSRIs and movement disorders has been previously documented.3,4 Tremor has been listed as the most common movement disorder side effect of SSRIs.5 Stuttering has also been shown to be associated with SSRI use. Symptoms typically resolve when the agent is discontinued.6
Stuttering can be developmental or acquired. Developmental stuttering presents during speech development in childhood at ages 3-9. Acquired stuttering is multifactorial and can be further divided into psychogenic and neurogenic categories. Neurogenic stuttering occurs after brain injuries or damage from drugs and toxins, while psychogenic stuttering appears in patients with psychiatric illness or emotional trauma.
The differential diagnosis of adult-onset stuttering includes traumatic brain injury, brain mass, stroke, epilepsy, drug abuse, psychogenic, medication induced, or chronic depression. Our laboratory and radiology results as well as a thorough history narrowed this list to medication induced stuttering. A literature review of drug-induced stuttering showed three publications describing stuttering caused by sertraline.7 Other medications associated with stuttering include theophylline8 antipsychotics,9 tricyclic antidepressants,10 memantine,11 and pregabalin.12 Additional speech changes can also be attributed to medication use. For example, topiramate, used in the treatment of seizure disorders and migraine, has been associated with echolalia13 and is known to negatively affect verbal fluency.14
It has been hypothesized that elevated dopamine levels contribute to stuttering.15 This hypothesis is further reinforced by findings of dopamine blocking medications used in successfully treating stutters.15 SSRIs, by definition, increase serotonin levels, but they also have been found to increase dopamine levels and play a role in movement regulation at the level of the basal ganglia. Interestingly, a prior study utilizing numerous SSRIs resulted in sertraline as the only medication in its class that was able to cause inhibition of dopamine reuptake in the striatum and nucleus accumbens.16 These findings, along with the temporal association of the stutter in our patient, further strengthen the working diagnosis of medication-induced stuttering. A very similar presentation with the same dosages was also documented in 1994.17
Case Resolution
After clinical assessment and workup in the emergency department, the patient was admitted to the hospital. The patient presented to the emergency department late in the evening. They were admitted overnight for monitoring, further imaging and neurology evaluation. The consulting neurologist noted the only abnormalities on neurologic examination were an apparent stutter and titubation with extension of the neck.
The patient’s presentation was determined to be secondary to a medication side effect. The hospitalist and neurology team agreed to the plan of titrating the sertraline dose back to the previously tolerated dose of 50 mg daily. The patient was discharged from the hospital the next day in stable condition with instructions to follow up with her psychiatrist.
Take-Home Points
- Commonly prescribed medications such as SSRIs may be a potential cause of movement disorders and speech disturbance. These unusual symptoms present a diagnostic challenge for the ED physician, and although not life-threatening, they can severely affect a patient’s quality of life.
- Female patients with seemingly vague neurologic complaints are often dismissed as having a behavioral component to their presentation.18,19
- Women with ischemic strokes are less likely to have their symptoms recognized,20 to undergo diagnostic testing, or to see a specialist.21
This report encourages emergency physicians to reflect on implicit biases and the tendency to overlook or downplay atypical neurologic symptoms. It also stresses the importance of taking a thorough and complete medication history.
References
- Friedman JH. Movement disorders induced by psychiatric drugs that do not block dopamine receptors. Parkinsonism Relat Disord. 2020 Oct;79:60-64. doi: 10.1016/j.parkreldis.2020.08.031. Epub 2020 Aug 26. PMID: 32871538.
- Leo RJ. Movement disorders associated with the serotonin selective reuptake inhibitors. J Clin Psychiatry. 1996 Oct;57(10):449-54. doi: 10.4088/jcp.v57n1002. PMID: 8909330.
- Gerber PE, Lynd LD. Selective serotonin-reuptake inhibitor-induced movement disorders. Ann Pharmacother. 1998 Jun;32(6):692-8. doi: 10.1345/aph.17302. PMID: 9640489.
- Dixit S, Khan SA, Azad S. A Case of SSRI Induced Irreversible Parkinsonism. J Clin Diagn Res. 2015 Feb;9(2):VD01-VD02. doi: 10.7860/JCDR/2015/11394.5583. Epub 2015 Feb 1. PMID: 25859504; PMCID: PMC4378786.
- Hirsch, M., & Birnbaum, R. J. (n.d.). Selective serotonin reuptake inhibitors: Pharmacology, administration, and side effects. UpToDate. https://www.uptodate.com/contents/selective-serotonin-reuptake-inhibitors-pharmacology-administration-and-side-effects#H399780694
- Di Rocco A, Brannan T, Prikhojan A, Yahr MD. Sertraline induced parkinsonism. A case report and an in-vivo study of the effect of sertraline on dopamine metabolism. J Neural Transm (Vienna). 1998;105(2-3):247-51. doi: 10.1007/s007020050053. PMID: 9660102.
- Nikvarz N, Sabouri S. Drug-induced stuttering: A comprehensive literature review. World J Psychiatry 2022; 12(2): 236-263 [PMID: 35317340 DOI: 10.5498/wjp.v12.i2.236]
- Movsessian P. Neuropharmacology of theophylline induced stuttering: the role of dopamine, adenosine and GABA. Med Hypotheses. (2005) 64:290–7. 10.1016/j.mehy.2004.07.026
- Bär KJ, Häger F, Sauer H. Olanzapine- and clozapine-induced stuttering. A case series. Pharmacopsychiatry. 2004 May;37(3):131-4. doi: 10.1055/s-2004-818992. PMID: 15179972.
- Hays P. Bethanecol chloride in treatment of stuttering. Lancet. 1987 Jan 31;1(8527):271. doi: 10.1016/s0140-6736(87)90086-9. PMID: 2880084.
- Alaghband-Rad J, Nikvarz N, Tehrani-Doost M, Ghaeli P. Memantine-induced speech problems in two patients with autistic disorder. Daru. 2013 Jul 2;21(1):54. doi: 10.1186/2008-2231-21-54. PMID: 23819879; PMCID: PMC3711986.
- Mancano MA. ISMP Adverse Drug Reactions: Pregabalin-Induced Stuttering Nitroglycerine-Induced Bradycardia Progressing to Asystole Minocycline-Induced DRESS Leading to Liver Transplantation and Type 1 Diabetes Increased Risk of Vertebral Fractures in Women Receiving Thiazide or Loop Diuretics Gambling Disorder and Impulse Control Disorder with Aripiprazole. Hosp Pharm. 2017 Apr;52(4):253-257. doi: 10.1310/hpj5204-253. PMID: 28515502; PMCID: PMC5424827.
- Akil E., Alp R., Atli A., Acar A., Ozdemier H. H. (2014). A case of echolalia in a topiramate induced patient with epilepsy. Journal of Clinical and Experimental Investigations, 5(4), 620–622. 10.5799/ahinjs.01.2014.04.0472
- Witt JA, Elger CE, Helmstaedter C. Impaired verbal fluency under topiramate--evidence for synergistic negative effects of epilepsy, topiramate, and polytherapy. Eur J Neurol. 2013 Jan;20(1):130-7. doi: 10.1111/j.1468-1331.2012.03814.x. Epub 2012 Jul 25. PMID: 22827489.
- Maguire GA, Nguyen DL, Simonson KC, Kurz TL. The Pharmacologic Treatment of Stuttering and Its Neuropharmacologic Basis. Front Neurosci. 2020 Mar 27;14:158. doi: 10.3389/fnins.2020.00158. PMID: 32292321; PMCID: PMC7118465.
- Kitaichi Y, Inoue T, Nakagawa S, Boku S, Kakuta A, Izumi T, Koyama T. Sertraline increases extracellular levels not only of serotonin, but also of dopamine in the nucleus accumbens and striatum of rats. Eur J Pharmacol. 2010 Nov 25;647(1-3):90-6. doi: 10.1016/j.ejphar.2010.08.026. Epub 2010 Sep 9. PMID: 20816814.
- Makela, Eugene H.; Sullivan, Pamela MD; Taylor, Michael MD. Sertraline and Speech Blockage. Journal of Clinical Psychopharmacology 14(6):p 432, December 1994.
- Ballering AV, Muijres D, Uijen AA, Rosmalen JGM, Olde Hartman TC. Sex differences in the trajectories to diagnosis of patients presenting with common somatic symptoms in primary care: an observational cohort study. J Psychosom Res. 2021 Oct;149:110589. doi: 10.1016/j.jpsychores.2021.110589. Epub 2021 Jul 31. PMID: 34385033
- McLoughlin C et al. Functional neurological disorder is a feminist issue. J Neurol Neurosurg Psychiatry. 2023 Oct;94(10):855-862. doi: 10.1136/jnnp-2022-330192. Epub 2023 Mar 28. PMID: 36977553; PMCID: PMC10511956.
- Govindarajan P, Friedman BT, Delgadillo JQ, Ghilarducci D, Cook LJ, Grimes B, McCulloch CE, Johnston SC. Race and sex disparities in prehospital recognition of acute stroke. Acad Emerg Med. 2015 Mar;22(3):264-72. doi: 10.1111/acem.12595. Epub 2015 Feb 25.
- Bruce SS, Merkler AE, Bassi M, Chen ML, Salehi Omran S, Navi BB, Kamel H. Differences in Diagnostic Evaluation in Women and Men After Acute Ischemic Stroke. J Am Heart Assoc. 2020 Mar 3;9(5):e015625.



